How Cancer Cells Evade the Immune System
Cancer cells employ numerous tactics to avoid detection and attack by the immune system. These include decreasing the expression of surface proteins that would identify the cell as abnormal, suppressing immune cells through release of cytokines and recruitment of regulatory T-cells, activating immune checkpoint pathways like PD-L1 to shut down cytotoxic T-cells, hijacking immune-suppressive cells like tumor-associated macrophages to create tolerance, masking tumor antigens through shedding decoys, forming physical barriers against immune cell infiltration, leveraging properties of the tumor microenvironment like low pH and hypoxia to blunt immune function, and enhancing resistance pathways to withstand immune assault. The sum of these evasive maneuvers creates an immunosuppressive tumor niche that enables immune escape. However, understanding these mechanisms has opened doors for immunotherapy approaches able to counteract malignant immune evasion.
Executive Summary
Cancer cells have developed multiple ways to evade the immune system: This is a complex process that has evolved over time. Cancer cells that are better at evading the immune system are more likely to survive and reproduce, leading to tumors that are experts at hiding from our body's defenses.
Downregulation of surface markers: Cancer cells reduce proteins like MHC molecules on their surface. These proteins usually act like flags that signal to immune cells that something is wrong. By lowering these flags, cancer cells become less visible to patrolling immune cells. It's as if they're changing their appearance to blend in with normal cells.
Immunosuppressive cytokines: Cancers release chemicals called cytokines that weaken nearby immune cells. These chemicals can make immune cells less active or even cause them to die. It's like cancer is creating a fog that confuses and weakens the immune system in its immediate area.
Recruitment of regulatory T cells (Tregs): Tregs are a type of immune cell that normally prevent autoimmune diseases by suppressing immune responses. Cancer cells attract these Tregs and use them as bodyguards. The Tregs then suppress other immune cells that might attack the cancer, creating a protective bubble around the tumor.
Checkpoint molecules: Our immune system has natural "brakes" to prevent it from attacking our own body. Cancer cells exploit these brakes, known as checkpoints. They produce proteins that activate these checkpoints, essentially telling immune cells to stand down. It's like cancer cells have found the off switch for the immune response.
Myeloid cell effects: Myeloid cells, including macrophages, are usually first responders of the immune system. However, cancer can reprogram these cells to help it instead. These corrupted cells, known as tumor-associated macrophages (TAMs), can suppress other immune cells and even help the cancer grow and spread.
Metabolic disruption: Cancer cells grow rapidly and consume a lot of nutrients. This creates an environment around the tumor that's low in the resources immune cells need to function. Additionally, cancer cells produce waste products that can be toxic to immune cells. It's like the cancer is both starving and poisoning the immune cells in its vicinity.
Resistance to cell death: Normally, when cells become abnormal, they undergo a process of programmed cell death called apoptosis. Cancer cells develop ways to resist this process. They can decrease the receptors that receive death signals, or increase proteins that promote survival. This makes them much harder for the immune system to kill.
Immunosuppressive exosomes: Exosomes are tiny vesicles that cells use to communicate with each other. Cancer cells release exosomes packed with molecules that suppress the immune response. These exosomes can travel some distance, allowing the cancer to influence immune cells that aren't in direct contact with the tumor.
The article provides a more technical explanation of each mechanism: For those with a scientific background, the article delves into the molecular details of these processes. This includes specific proteins and signaling pathways involved in each mechanism of immune evasion.
Earlier in this article we have looked at how cancer cells evade the immune system. We have covered this same material in both a very simple way and then in a somewhat more detailed way. In this segment, going to look at the very same information from a much more technical view. For many of you reading this, this will be likely well beyond your understanding. Don't feel that you have to somehow dig through this in order to understand cancer nor in order to make good choices. Most of you will likely just skip this section and that's just fine. We put this here for those of you that have a greater level of training or for whatever reason you want to dig deeply into the specifics of how this takes place. If you're one of those people, we hope that this provides you what you need.
Upcoming Sections
Downregulation of surface markers
Cancer cells reduce expression of MHC and antigen molecules, making it harder for immune cells like T cells to recognize them as foreign.
Recruitment of Tregs
Regulatory T cells (Tregs) are recruited by tumors and suppress the activity of cytotoxic T cells that could attack the cancer.
Myeloid cell effects
Cancer cells attract immunosuppressive myeloid cells like tumor-associated macrophages which can inhibit T cell function.
Resistance to cell death
Cancer cells mutate to avoid immune-mediated apoptosis and decrease surface presentation of death receptors like Fas.
Immunosuppressive cytokines
Tumors secrete cytokines like IL-10, TGF-beta, and VEGF that broadly inhibit immune cells in the tumor microenvironment.
Checkpoint molecules
Cancer cells express PD-L1 which binds PD-1 on T cells, putting the brake on T cell killing. Other checkpoints like CTLA-4 also dampen the immune response.
Metabolic disruption
The chaotic tumor metabolism can deplete nutrients needed by T cells and produce toxic metabolites that impair T cells.
Immunosuppressive exosomes
Vesicles secreted by tumors contain substances like adenosine and TGF-beta that suppress T cell activity in the local environment.
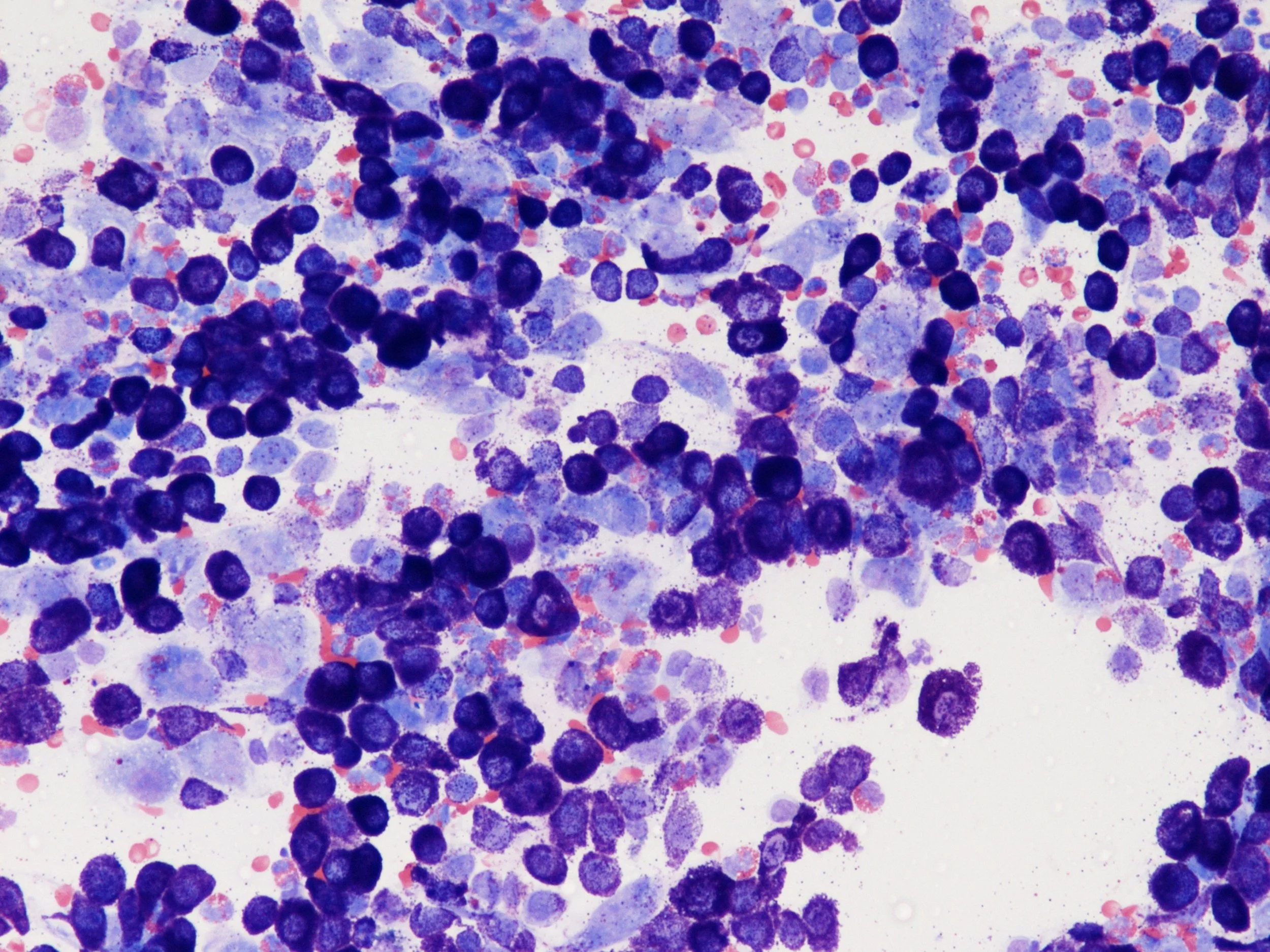
Downregulation of surface markers
A key way cancers evade the immune system is by reducing the expression of certain molecules on their cell surface that allow immune cells like T cells to recognize them as foreign or dangerous. Two important types of surface molecules that cancer cells downregulate are MHC molecules and tumor antigens.
Major histocompatibility complex (MHC) molecules display fragments of proteins from inside the cell on the cell surface. T cells survey these MHC-peptide complexes to determine if they are normal "self" proteins or foreign "non-self" proteins that may be a threat. Cancer cells decrease the levels of MHC class I molecules on their surface, which prevents display of tumor antigens to T cells. Tumor antigens are proteins produced by cancer cells that would normally provoke an immune response if detected. By downregulating MHC class I, cancer cells prevent T cell recognition of these tumor antigens. CD8 cytotoxic T cells in particular rely on interacting with MHC class I to identify infected or transformed cells to kill.
In addition to reducing MHC class I, cancer cells also decrease expression of co-stimulatory molecules like CD80 and CD86 needed for proper T cell activation after antigen recognition. This two-pronged downregulation of both antigen presentation (MHC class I) and co-stimulation results in ineffective T cell surveillance of tumors. Understanding how cancers achieve "immune escape" through altering expression of MHC, tumor antigens, and co-stimulatory molecules has led to new immunotherapeutic strategies, such as checkpoint inhibitors, aimed at restoring impaired anti-tumor immune responses.
Immunosuppressive cytokines
In addition to downregulating surface proteins, cancer cells also evade immune detection by releasing certain inhibitory signaling molecules called cytokines into their surrounding microenvironment. Key immunosuppressive cytokines produced by many tumors include interleukin-10 (IL-10), transforming growth factor beta (TGF-β), and vascular endothelial growth factor (VEGF).
IL-10 is an anti-inflammatory cytokine that impairs the function of several immune cells involved in anti-tumor immunity. It inhibits the maturation of dendritic cells as well as the activation of T cells and natural killer cells. IL-10 may also promote immunosuppressive regulatory T cells (Tregs) in the tumor microenvironment.
TGF-β has broad immunosuppressive effects, blocking the proliferation, differentiation, and activity of T cells, NK cells, and other immune cells. It also enhances the function of immunosuppressive Tregs. High TGF-β levels in the tumor microenvironment are associated with immune evasion.
VEGF is best known as a promoter of tumor angiogenesis, but it also exhibits immunosuppressive properties. VEGF signaling inhibits the maturation and activation of dendritic cells. It also impairs lymphocyte development and trafficking into the tumor.
Together, these cytokines create an immunosuppressive milieu around the tumor that prevents immune cells from mounting an effective anti-cancer response. Understanding this cytokine-mediated inhibition has led to new immunotherapies like cytokine-blocking antibodies and engineered T cells resistant to cytokine effects.
Immunosuppressive regulatory T cells (Tregs)
Regulatory T cells (Tregs) are a subpopulation of T cells that act to suppress immune responses and promote tolerance to self-antigens. Cancer cells have devised ways to co-opt Tregs to create an immunosuppressive microenvironment that shields the tumor from immune attack. Tregs express certain receptors like CCR4 and CTLA-4 that allow them to be recruited into the tumor in response to chemokines like CCL22. Binding of CTLA-4 on Tregs to CD80/CD86 on dendritic cells also enhances Treg immunosuppressive activity. Once within the tumor, Tregs inhibit the activation and effector functions of CD4+ helper T cells and CD8+ cytotoxic T cells that could potentially recognize and kill cancer cells.
Key mechanisms of Treg-mediated immune suppression include:
Secretion of inhibitory cytokines like IL-10, IL-35, and TGF-beta.
Metabolic disruption of effector T cells by depletion of IL-2 and other metabolites.
Expression of CTLA-4 which outcompetes CD28 costimulation on T cells.
Cytotoxic killing of antigen-presenting dendritic cells.
By promoting Treg recruitment and activation, tumors create an environment rich in immune-suppressive cells that prevents an immune response capable of destroying the cancer. Checkpoint immunotherapy blocking CTLA-4 aims to reduce Treg immunosuppression and reactivate anti-tumor immunity. Depleting Tregs is also being explored as a potential therapeutic strategy.
Checkpoint molecules
T cells have built-in "checkpoints" or inhibitory pathways that normally maintain self-tolerance and prevent excessive immune activation. Cancer cells exploit these regulatory pathways by expressing checkpoint ligands that bind to receptors on T cells, effectively putting the "brakes" on anti-tumor T cell activity. One major checkpoint pathway hijacked by tumors is the PD-1/PD-L1 axis. PD-L1 is a ligand expressed on many cancer cells. It binds to the PD-1 receptor on T cells, triggering an inhibitory signaling cascade that reduces T cell proliferation, survival, and effector functions. Engagement of PD-1 by PD-L1 essentially dampens or shuts down T cell attacks against the tumor.
In addition to PD-1/PD-L1, cancer cells also exploit other T cell checkpoint pathways like CTLA-4. CTLA-4 is a receptor on T cells that outcompetes the costimulatory receptor CD28 for binding to CD80/CD86 on antigen presenting cells. CTLA-4 binding transmits inhibitory signals to shut down T cell activation. Many tumors upregulate CD80/CD86 to augment CTLA-4 mediated suppression.
Blocking antitumor T cell checkpoint pathways like PD-1 and CTLA-4 has become a major immunotherapy strategy. Checkpoint inhibitor drugs like pembrolizumab and ipilimumab release the "brakes" on T cells, allowing renewal of cancer-killing immunity.
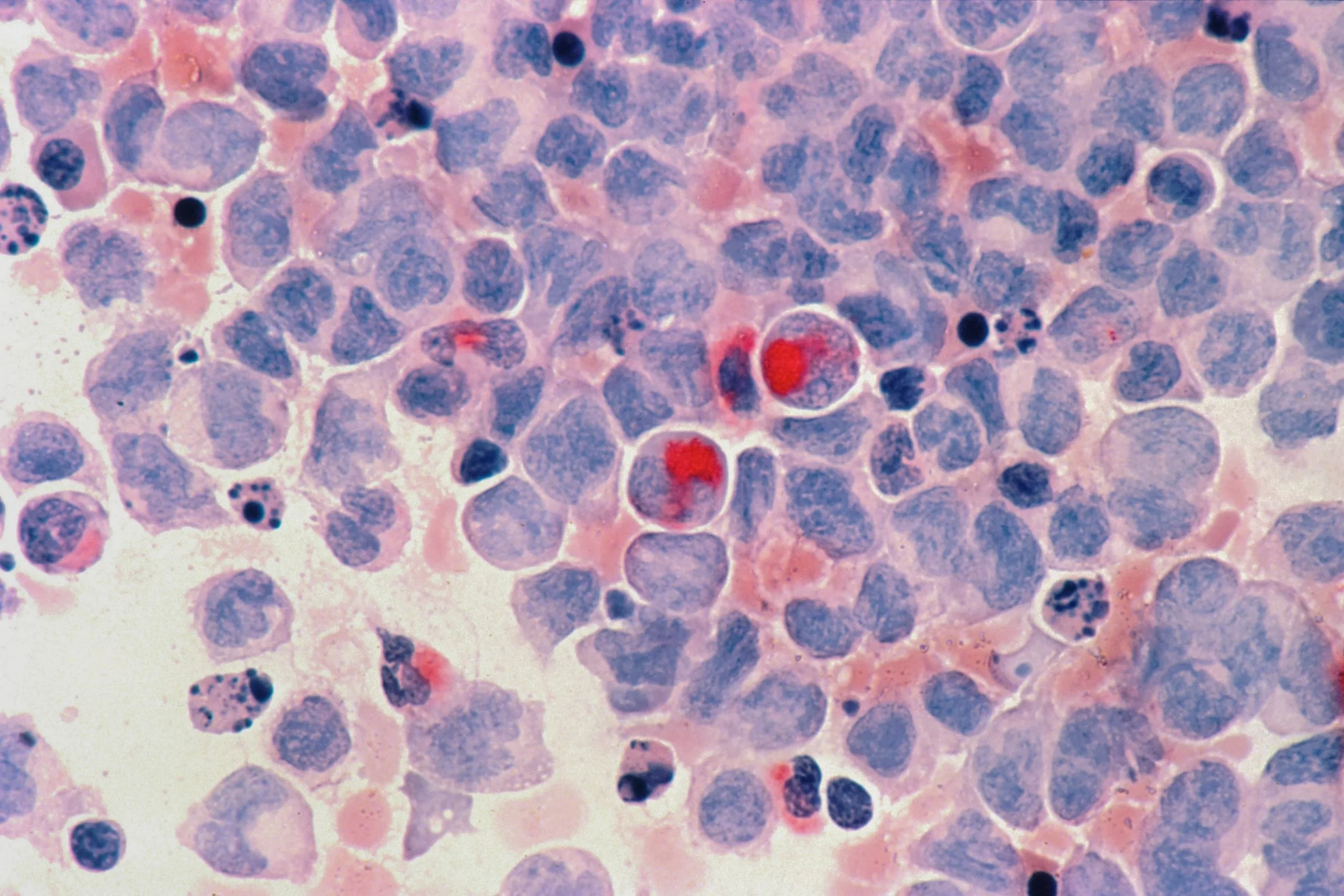
Myeloid cells like tumor-associated macrophages (TAMs)
In addition to the adaptive immune system, tumors also exploit and corrupt cells of the innate immune system to create an immunosuppressive microenvironment. An important example is tumor-associated macrophages (TAMs). Macrophages are innate myeloid cells that normally activate immune responses against pathogens. However, macrophages exposed to the tumor microenvironment undergo changes that reprogram them into TAMs with immunosuppressive properties. Cancer cells secrete chemokines like CCL2 that recruit monocytes from the bloodstream into the tumor, where growth factors like CSF-1 and IL-10 polarize them into TAMs. TAMs in turn release various cytokines and mediators that inhibit CD8+ cytotoxic T cells and CD4+ helper T cells.
Mechanisms of TAM-mediated T cell suppression include:
Depletion of metabolites like glucose and arginine needed for T cell function
Production of immune-suppressive lactate
Expression of PD-L1 which activates PD-1 checkpoint on T cells
Secretion of cytokines like IL-10 and TGF-β
Targeting TAMs with therapies like anti-CSF-1R aims to reactivate anti-tumor immunity. Overall, re-educating immunosuppressive innate immune cells in the tumor microenvironment remains an important goal for cancer immunotherapy.
Metabolic disruption
The disorganized and rapid metabolism of cancer cells creates a toxic microenvironment that metabolically deprives immune cells of key nutrients and functional molecules. This metabolic disruption is another strategy tumors use to suppress anti-cancer immune responses. Tumors utilize aerobic glycolysis (the Warburg effect) which involves high uptake of glucose and production of lactate. This creates competition for glucose, starving tumor-infiltrating lymphocytes (TILs) of the glucose needed for their activation and effector functions. In addition, the acidic conditions due to lactate secretion inhibit T cell proliferation and cytokine production. Lactate itself can also restrain T cell responses through effects on signaling pathways like mTOR. Besides glucose depletion, tumors also exhibit increased demand for amino acids like tryptophan. The loss of tryptophan inhibits T cell activation, likely by disrupting mTOR signaling. Similarly, arginine depletion by myeloid cells in the tumor microenvironment blunts T cell function.
Overall, the nutrient-deprived and metabolite-rich conditions of the tumor block metabolic pathways essential for anti-tumor T cell immunity. Understanding these disruptions has led to emerging therapies like glucose transport inhibitors as well as engineered T cells resistant to tumor-driven metabolic stresses.
Resistance to cell death
The immune system deploys several mechanisms to directly induce programmed cell death (apoptosis) of cancer cells, including expression of death receptors and release of cytotoxic granules. However, tumors evolve strategies to resist immune-mediated apoptosis and evade elimination. One way tumors become resistant is by decreasing surface expression of death receptors like Fas (CD95). Binding of Fas ligand (FasL) on cytotoxic T cells to Fas normally triggers apoptosis. By downregulating Fas, cancer cells avoid this apoptotic signaling.
In addition, tumors upregulate expression of anti-apoptotic proteins like Bcl-2 that inhibit the intrinsic apoptotic pathway. This allows cancer cells to withstand both extrinsic and intrinsic pro-apoptotic signals. Cancer cells also reduce surface presentation of TRAIL receptors while increasing decoy receptors, enabling avoidance of TRAIL-induced apoptosis by natural killer cells. Moreover, tumors develop mutations in the p53 tumor suppressor pathway, disabling a major regulator of apoptosis. Loss of p53 function allows cancer cells to survive despite genomic instability and immune attack.
Re-sensitizing resistant tumors to immune cell-mediated cytotoxicity remains a major goal for immunotherapy. For instance, some strategies aim to overexpress death receptors like Fas or counteract anti-apoptotic proteins like Bcl-2.
Immunosuppressive exosomes
In addition to soluble factors, tumors also release extracellular vesicles known as exosomes that transport immunosuppressive cargo to nearby immune cells. These tumor-derived exosomes are an important mechanism contributing to the inhibitory microenvironment. Exosomes are lipid-encased vesicles encapsulating proteins, nucleic acids, metabolites, and other biomolecules. Cancer cells secrete large quantities of these nanoparticles, which act as intercellular messengers. Tumor-derived exosomes carry immunosuppressive payloads that alter the function of surrounding immune cells. For example, exosomes contain metabolites like adenosine that broadly inhibit T cell activation and effector responses when uptaken. They also contain immunosuppressive cytokines like TGF-β which represses both innate and adaptive anti-tumor immunity. In addition, exosomes display PD-L1 on their surface, interacting with PD-1 on T cells to induce dysfunction.
Overall, the secreted exosomes essentially act as immunosuppressive "drones" that disseminate inhibitory cargos throughout the tumor microenvironment. Understanding this liquid-phase communication network is leading to cutting-edge therapies like engineered exosome "biologics" aimed at reprogramming the immune landscape.
https://genesdev.cshlp.org/content/32/19-20/1267.full https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-022-01138-3 https://genesdev.cshlp.org/content/32/19-20/1267.full https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-022-01138-3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4493378/ https://www.tandfonline.com/doi/epdf/10.1517/14712598.5.4.463?needAccess=true https://www.sciencedirect.com/science/article/abs/pii/S0378512217305315 https://www.mdpi.com/1422-0067/21/1/157