Mutated Stem Cells
Cancer metastasis refers to the spread of cancer cells from a primary tumor to distant sites in the body. It represents one of the most life-threatening aspects of cancer progression and is responsible for the majority of cancer deaths worldwide. Despite extensive research, the metastatic process remains incredibly complex and many crucial questions persist.
Executive Summary
Cancer metastasis is the spread of cancer cells from the original tumor to other parts of the body. It's responsible for most cancer deaths worldwide. Understanding why some cancer cells can spread while others can't is a major challenge for researchers.
Cancer stem cells (CSCs) are a special subset of cancer cells that can self-renew and give rise to different types of cancer cells. They're thought to be responsible for tumor growth, therapy resistance, and metastasis. CSCs can survive many standard cancer treatments, which is why cancers often come back.
CSCs were first discovered in leukemia in the 1990s. Since then, they've been found in many solid tumors like breast, brain, and colon cancers. CSCs can be identified and isolated using special markers and techniques.
CSCs have unique abilities that make them dangerous. They can divide indefinitely, produce different types of cancer cells, resist therapies, evade the immune system, and promote blood vessel growth in tumors. These abilities allow CSCs to drive tumor growth and spread.
The origin of CSCs is still debated. They might come from normal stem cells that acquired mutations, or from regular cancer cells that gained stem-like properties. Understanding where CSCs come from could help develop better treatments.
CSCs are thought to be key players in cancer metastasis. They can survive in the bloodstream, settle in new organs, and start new tumors. Targeting CSCs could be a way to prevent or treat metastasis, which is the main cause of cancer deaths.
Treating CSCs is challenging because they're resistant to many standard therapies. Researchers are looking for ways to specifically target CSCs, such as blocking their unique signaling pathways or using their surface markers to deliver drugs.
Several natural compounds show promise in targeting CSCs. These include curcumin (from turmeric), resveratrol (found in grapes), EGCG (from green tea), quercetin (in many fruits and vegetables), and sulforaphane (from broccoli and other cruciferous vegetables). These compounds can affect CSCs in multiple ways, potentially making them less likely to survive and spread.
Using natural compounds to target CSCs could have advantages. They often have fewer side effects than traditional chemotherapy and can work in multiple ways to attack CSCs. However, more research is needed to figure out the best ways to use these compounds in cancer treatment.
While research on CSCs and natural compounds is promising, there are still challenges. We need to learn more about how to deliver these compounds effectively in the body and how to combine them with other treatments. Clinical trials are needed to see if these approaches work in cancer patients.
Background on Cancer Metastasis
A key issue is identifying why some cancer cells are able to successfully metastasize while others remain localized. Metastasis is an inefficient process - cells must accomplish a sequential series of steps including breaking away from the primary tumor, invading the circulatory system, surviving transit, adhering at a distant secondary site, and establishing growth of secondary tumors. It’s estimated that less than 0.1% of circulating tumor cells ultimately succeed in forming metastases. This suggests that only a small subpopulation of cancer cells possess the full necessary machinery and capabilities required for the metastatic cascade. Determining the origins of metastatic ability and the underlying mechanisms driving it continues to challenge researchers.
Another central question is the timing of metastasis and patterns of spread. Dissemination of metastatic cells may occur early in tumor progression or later following additional genetic changes. The patterns of circulation and sites of eventual secondary growth also vary between cancer types based on factors that are not fully defined. Bone, liver, lung and brain are among the most common secondary sites, however the key molecular and cellular determinants of this organ-specific tropism remain obscure.
Significant debate also centers around the cellular origins of metastatic deposits. Traditionally, it was thought they arise from the bulk of a genetically heterogeneous primary tumor. However, emerging evidence points to specialized subpopulations of cells that drive metastasis. In particular, cancer stem cells have come under scrutiny as potential metastasis-initiating cells that propagate secondary growths. This highlights the importance of understanding interactions between metastatic patterns and the underlying genetics, epigenetics and microenvironmental cues influencing tumor cells.
From a clinical perspective, preventing and treating metastasis represents an urgent priority as it accounts for the high mortality rates of malignancies like breast, prostate, lung and colon cancer. Yet most therapeutic approaches target bulk tumor cells rather than embolic metastatic seeds, which may explain failures to improve patient survival substantially. Ultimately, new therapies will rely upon unlocking the biological determinants and molecular pathways that dictate a cancer cell’s metastatic potential versus remaining localized.
In summary, elucidating the mechanisms that enable metastasis to occur efficiently in some cells versus others remains a multifaceted problem confounded by cancer's heterogeneity in space and time. Myriad interconnected factors related to tumor evolution, the microenvironment, genetics, cell signaling and more influence metastatic success. As researchers continue unraveling these mysteries, opportunities to predict, prevent and eradicate deadly metastatic disease may emerge, offering hopes of reducing cancer’s lethal toll.
Introduction to Cancer Stem Cells and their Implications for Metastasis
The origins of the cancer stem cell (CSC) concept trace back to observations in the 1960s that only a minority of leukemia cells were capable of proliferating extensively upon transplantation into mice. This implied leukemia propagation was driven by a subset with enhanced proliferative potential.
In the 1990s and 2000s, Dr. John Dick and colleagues made seminal observations while studying acute myeloid leukemia (AML). They demonstrated through xenotransplantation assays that only an extremely small fraction of AML cells could successfully transfer disease into mice. Additionally, these cells could be serially passaged, proving self-renewal ability. Dr. Dick termed these cells "leukemia stem cells" given their stem-like properties.
This pioneering work laid the foundation for the CSC model, which posits that many cancers are hierarchically organized with a specialized subpopulation of stem-like cells dictating propagation and growth. This paradigm was initially met with skepticism, as the prevailing stochastic model of tumorigenesis proposed all cancer cells possess equal tumorigenic potential.
The CSC concept gained significant traction in 2003 when Dr. Michael Clarke and colleagues isolated a subpopulation of breast cancer cells showing elevated tumor-initiating capacity upon transplantation into mice. These cells also expressed stem cell surface markers, providing further evidence of a CSC hierarchy.
Subsequently, many researchers isolated and studied CSC populations from diverse solid tumor types, including brain, colon, pancreatic, prostate and others. Their self-renewal and tumor propagation potential was serially confirmed through passaging in xenograft models. Additionally, correlations between CSC markers and poorer clinical outcomes emerged, underscoring their clinical relevance.
By the late 2000s, CSCs were widely implicated as key orchestrators of tumor growth, metastasis, therapy resistance and relapse. Ongoing efforts have focused on unraveling their molecular regulation, interactions with the microenvironment, evolution during cancer progression, and therapeutic targeting. Further dissecting CSC biology remains imperative for conquering deadly metastases and recurrences.
The CSC model thus emerged over decades of incremental discoveries illuminating the hierarchical organization and stem-like properties of minority cancer cell subpopulations. Their identification catalyzed a paradigm shift that continues guiding metastatic and therapeutic research.
Identification and Isolation of Cancer Stem Cells
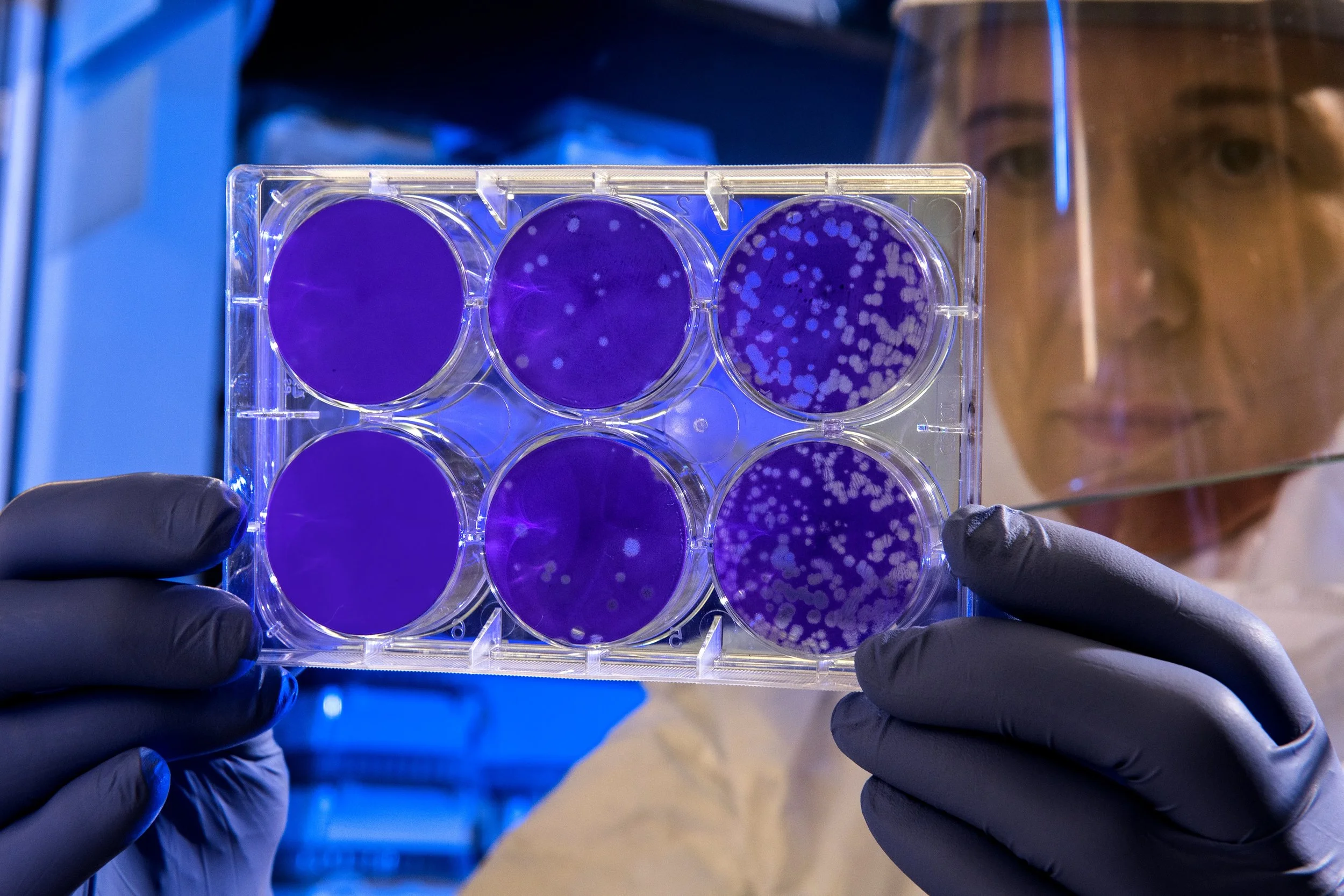
Multiple experimental approaches enable isolation and characterization of CSCs from tumor samples. Fluorescence-activated cell sorting (FACS) can segregate cells expressing putative stem cell markers like CD44, CD133, EPCAM, CD24, CD90, and ALDH1, which are then validated functionally. Anchorage-independent culture selects for self-renewing CSCs capable of proliferating as undifferentiated spheroids in serum-free medium, unlike differentiated cells. High ALDH enzyme activity, measured via Aldefluor assays, also marks stem-like cells. In vivo lineage tracing in mouse models allows dynamically tracking CSC progeny during tumor progression. These strategies all facilitate isolating CSCs for characterization.
Xenotransplantation - the Gold Standard Assay
The gold standard methodology to prove stemness involves transplanting candidate CSCs into immunodeficient mice. CSCs capable of tumor initiation and self-renewal will propagate new tumors that histologically resemble the original malignancy. Serial transplantation through multiple generations demonstrates self-renewal. Limiting dilution analysis quantifies the frequency of CSCs based on tumor-propagating ability. As few as 100 CSCs can recapitulate the parent tumor whereas hundreds of thousands of bulk cancer cells fail to form tumors, powerfully demonstrating stemness.
Headline
Self-Renewal
The capability for relentless self-renewal is a cardinal feature defining cancer stem cells (CSCs). Whereas most tumor cells possess a limited proliferative potential before undergoing senescence, CSCs can divide without limit. This grants CSCs a form of cellular “immortality” akin to normal tissue stem cells.
CSCs have the flexibility to self-renew through either symmetric or asymmetric cell division. When a CSC divides symmetrically, it produces two identical daughter CSCs. This doubles the stem-like cell pool to drive tumor expansion. Alternatively, asymmetric division generates one new CSC and one differentiated cell. This maintains the CSC population while also providing a continual source of cells contributing to overall tumor bulk.
By harnessing these self-renewal pathways, a small starting population of CSCs in a tumor can spawn boundless numbers of malignant progeny over time. This perpetual regenerative ability serves as the engine enabling sustained primary and metastatic tumor growth. From a clinical standpoint, the fact that CSCs resist many standard therapies means they can persist and continue driving regeneration after treatment.
Differentiation
On top of self-renewal, CSCs are multipotent - they can differentiate down multiple lineages to generate phenotypically diverse cancer cell types. This accounts for the conspicuous cellular heterogeneity within tumors, which are mosaics of cells with varied functions and markers rather than just uniform clones.
When a CSC divides asymmetrically, the daughter cell displaced from the CSC niche begins differentiating into a specialized tumor cell. Multipotent CSCs may generate a repertoire of cells including those contributing to the tumor stroma, vascular system, and immune microenvironment. This parallels the way normal organ development depends on stem cells spawning multiple specialized cell types.
The implications are clinically relevant. For one, if metastases arise from CSCs, their multipotency enables seeding metastases with heterogeneous compositions distinct from the primary tumor. Additionally, if therapies fail to eliminate multipotent CSCs, they can theoretically repopulate any malignant cell type lost to treatment through differentiation, thereby promoting relapse.
Deciphering the Role of Cancer Stem Cells in Tumor Recurrence and Metastasis
Elusive Therapy Resistance Mechanisms
A key challenge in oncology is that the majority of chemotherapies, radiation regimens, and even targeted drugs predominantly eliminate rapidly dividing tumor cells. However, they often fail to eradicate cancer stem cells. These cells exhibit a multitude of strategies to withstand treatment, including entering quiescence, upregulating drug efflux transporters, enhancing DNA repair activity, activating pro-survival signaling, and adopting slow-cycling or undifferentiated states.
For example, ABC transporters are membrane pumps that can eject drugs from cells before they take effect. Many CSCs overexpress these transporters, essentially creating resistance. CSCs may also overactivate DNA repair pathways to fix treatment-induced damage. And they seem to modulate cell death pathways to block apoptosis. Such mechanisms allow CSCs to persist like phantoms long after therapies ostensibly abolished the bulk tumor. Tragically, patients may then suffer recurrences or metastases years later arising from those tenacious CSCs. Finding approaches to eliminate or prevent their resistance is imperative.
CSCs as Architects of Metastasis
Regardless of their origins, CSCs are strongly implicated in disseminating and propagating metastatic tumors. Due to their tumor-seeding ability, CSCs likely orchestrate colonization of secondary sites after escaping the primary tumor. Therapies that fail to eliminate these cells may shrink tumors, yet ultimately prove futile if metastases later blossom from the few surviving CSCs. Animal studies reinforce this notion, with CSC transplantation successfully spawning metastases.
Additionally, the phenotypic plasticity and multipotency of CSCs raises the specter that metastases may exhibit different cellular compositions compared to the primary tumor. By differentiating, CSCs could populate new tumors with high cellular diversity distinct from the initial malignancy. This underscores the need to target CSCs rather than expect bulk tumor similarities.
Cancer researchers have recently devoted great attention to a subpopulation of cells known as cancer stem cells (CSCs). These cells, analogous to normal stem cells in organs, appear to initiate and sustain tumor growth. Evidence suggests CSCs demonstrate unique resistance to standard therapies, allowing them to drive recurrence after treatment. CSCs are also implicated as potential orchestrators of deadly tumor metastasis. However, many questions remain regarding their specific origins, evolution during cancer progression, and mechanisms underlying metastasis. Unlocking these mysteries may reveal vulnerabilities to finally outwit these cells.
Diverse Theories on Cancer Stem Cell Origins
Despite recognition of CSCs in many cancers, debate continues over their origins and evolution during tumorigenesis. One prominent model hypothesizes that CSCs arise from normal adult tissue stem cells that incurred transforming mutations. Tissue stem cells already possess extensive self-renewal ability, which cancer could essentially co-opt and dysregulate. However, evidence also suggests that fully differentiated cells can dedifferentiate back into CSC-like states in some cancers.
Adding complexity, the epithelial-to-mesenchymal transition (EMT) is known to confer both stem cell properties and mobility. Consequently, EMT has been proposed as a potential CSC origin, generating cells dually equipped for metastasis and tumor propagation. However, not all CSCs exhibit mesenchymal traits, implying additional origins must exist. Overall, research has yet to conclusively elucidate if distinct CSC subsets pre-exist early on, if stochastic transitions generate shifting CSC populations, or if microenvironmental cues prompt their emergence later.
Illuminating the Mysteries of Cancer Stem Cells
In summary, compelling evidence suggests we must destroy the therapy resistance and tumor-initiating abilities of cancer stem cells to achieve lasting cures. Yet mysteries linger regarding their origins, evolution, and detailed mechanisms enabling metastasis. Resolving these uncertainties will direct more precise therapeutic targeting. For instance, if CSCs arise stochastically, they may require approaches targeting the bulk tumor. But if they are predefined early on, selective CSC-directed therapies could offer hope. Similarly, delineating their metastasis pathways may reveal steps amenable to pharmacological blockade. While the cancer stem cell hypothesis has provided key insights, significant laboratory and clinical research remains vital to fully illuminate their sinister biology.
EMT and Motility
The epithelial-to-mesenchymal transition (EMT) is known to enable mobility, invasion and metastatic traits. It also imparts stem-like properties. Cells undergoing EMT may exhibit enhanced CSC phenotypes and functions, further linking acquisition of stemness and metastatic ability.
Therapy Resistance The therapy resistance of CSCs allows their survival after interventions that eliminate bulk tumor cells. This permits tumor regeneration from persistent CSCs. It also enables CSCs to disseminate prior to therapy and later manifest as metastasis after a dormancy period. Targeting CSC resistance pathways is critical.
To make matters more complex, when CSCs give rise to these secondary tumors, the new growths might not mirror the original tumor in terms of cell composition. This means that a treatment that was effective against the primary tumor might not necessarily work against metastases. Hence, there's a pressing need to develop therapeutic strategies that target the unique properties of CSCs, rather than just the bulk of the tumor.
In summary, accumulating evidence strongly implicates cancer stem cells as integral orchestrators of metastasis initiation and progression. Their stem-like properties including self-renewal, differentiation, therapy resistance, and tumor propagation capacity may directly enable critical steps of the metastatic cascade. Further biological insights into CSCs will pave the way for therapeutic strategies to prevent metastasis and thereby reduce cancer mortality.
How Normal Stem Cells and Cancer Stem Cells Compare
At first glance, normal stem cells in the body and cancer stem cells sound pretty alike - I mean, they both have “stem cell” right in the name! But when you look closer, there are some important distinctions between these two cell types. Understanding how they’re similar and different helps reveal why those cancer stem cells are so troublesome.
First, What Are Normal Stem Cells?
Let’s start with a quick primer on normal stem cells. These are special cells found in tissues and organs that have the incredible ability to develop into any of the specialized cells needed in that area. For example, blood stem cells in the bone marrow give rise to all types of blood cells. Meanwhile, skin stem cells generate new skin cells. Normal stem cells have a few other cool abilities too. First, they can copy themselves over and over through cell division, which is called self-renewal. They also can live for a very long time compared to their specialized progeny. These traits allow them to persist in the body as a source of new cells as needed.
Treatment Resistance
A signature feature of CSCs is increased resistance to standard cancer therapies. CSCs activate a range of programs to withstand chemotherapy, radiation, and even targeted drugs, including drug efflux pumps, DNA repair mechanisms, quiescence, survival signaling, and intrinsic resistance factors. This allows their persistence after therapy to drive recurrence and metastasis.
Immune Evasion
CSCs can effectively evade immune surveillance using myriad tactics. These include decreasing surface immunostimulatory proteins, secreting immunosuppressive cytokines, recruiting regulatory T cells, inducing checkpoint inhibitory pathways, and more. By camouflaging from immune responses, CSCs can persist undetected.
Now What Makes Cancer Stem Cells Different?
Cancer stem cells, or CSCs for short, are similar to normal stem cells in a few key ways. First, they can self-renew through cell division, allowing them to persist and accumulate in tumors. Second, they can give rise to a spectrum of different cell types, similar to normal stem cells producing specialized offspring. This accounts for the cellular diversity seen within tumors.
Importantly though, the ways CSCs use these normal stem cell-like abilities are distorted. While normal stem cells tightly regulate growth, CSCs divide uncontrollably. They can also drive continued tumor growth and progression when transplanted, unlike normal stem cells. Additionally, CSCs have their own bag of tricks not shared by normal stem cells. For example, they seem to resist cancer therapies, allowing them to survive treatment and drive recurrence. They also may have enhanced mobility and invasive abilities to spur metastasis. CSCs hijack some normal stem cell functions like self-renewal and differentiation, then twist them to serve their own tumorigenic agenda! Understanding their unique dark side is key to targeting these rogue cells.
Evidence for Cancer Stem Cells
Researchers have isolated subsets of cells from various cancer types that display surface markers and behaviors associated with stemness. When isolated based on marker expression and studied further, these cells demonstrate functional properties setting them apart from the bulk of the tumor cells. For instance, putative cancer stem cell populations can self-renew extensively and be serially passaged long-term in spheroid cultures and animal models, unlike regular tumor cells that lack this proliferative potential.
Additionally, cancer stem cells exhibit multipotency - they can differentiate into an array of other tumor cell types, mirroring the heterogeneity of the parent malignancy. Marker analysis confirms their progeny give rise to the diverse cells populating tumors. Moreover, when transplanted into immunodeficient mice at limiting dilutions, cancer stem cells form tumors more efficiently than other cancer cells, often initiating tumors at concentrations 1,000-fold lower. This highlights their superior tumor propagation capability.
Another signature feature of cancer stem cells is increased resistance to standard therapies like chemotherapy, radiation, and targeted drugs compared to other cancer cells. This aligns with clinical observations of treatment failures and cancer recurrence after therapy. Cancer stem cells also demonstrate enhanced migratory behavior indicative of metastatic potential, fitting with their hypothesized role as metastasis-initiating cells.
Across numerous studies and cancer types, these functional properties set cancer stem cells apart as a distinct self-renewing, tumor-propagating, and treatment-resistant subpopulation. Their conservation across patients further supports their unique function. Such complementary evidence substantiates the existence of cancer stem cells and their high relevance to tumor progression and therapeutic resistance.
Critical Capabilities of Cancer Stem Cells
Self-Renewal
The defining capability of cancer stem cells (CSCs) is unlimited self-renewal. Unlike regular cancer cells, CSCs can undergo symmetrical cell division repeatedly to expand the CSC pool. This perpetual regeneration allows unlimited tumor growth. CSCs can also divide asymmetrically to balance self-renewal with producing differentiated progeny. Persistence of the CSC niche sustains tumorigenesis long-term.
Differentiation
In addition to self-renewal, CSCs exhibit multipotency and can differentiate into the diverse malignant cell types comprising the overall tumor. This accounts for the conspicuous heterogeneity within tumors, which are mosaics of varied cancer cells rather than clonal expansions. The differentiation capacity of CSCs is pivotal for generating all necessary components that enable tumor viability and progression.
Induction of Angiogenesis
For tumors to grow and disseminate, they require a blood supply. CSCs potently induce angiogenesis - the formation of new blood vessels in tumors. They achieve this by secreting pro-angiogenic factors like VEGF that recruit endothelial cells to form vascular networks permeating tumors. Robust angiogenesis enables CSC maintenance and metastasis.
In summary, the specialized capabilities of unrestrained self-renewal, multipotency, treatment resistance, angiogenesis induction and immune system evasion enable CSCs to perpetuate tumors, catalyze progression, and defy therapies. Further research aims to fully elucidate CSC capabilities to reveal vulnerabilities for elimination.
Metastasis-Starting Cancer Stem Cells
Research shows that while cancer stem cells can reform tumors, only some may have the special skills to actually get the cancer spreading to new locations. These cells are called metastasis-initiating cancer stem cells.
Evidence shows specific groups of cancer stem cells are better at starting metastases versus just regrowing the first tumor when transplanted into mice. Also, cancer stem cells closer to the edges of a tumor or near blood vessels tend to be more metastatic, implying they are primed for travel.
What edge do metastasis-starting stem cells have? While regular cancer stem cells can rebuild the original tumor, the metastatic ones have extra powers to help the cancer spread, like being able to migrate better, survive in blood circulation, and specifically take root in other organs. Finding the keys to their spread-seeding abilities is important.
Metastatic cancer stem cells likely have increased migration capacity, can resist cell death while circulating unattached, and may have special proteins to dock specifically at future metastasis sites. Learning more about the tools these cells use to gain their metastatic powers could reveal ways to stop them.
Researchers can also compare the gene activity profiles of metastatic versus non-metastatic cancer stem cells to identify molecular signatures unique to the spreaders. This helps uncover the genes and pathways controlling the ability to kickstart metastases.
The takeaway is that while many cancer stem cells can reform tumors, a special subset seems to have the arsenal required to actually get the cancer spreading to distant sites. Learning as much as possible about this deadly subgroup could lead to big advances in preventing metastasis.
Implications of Metastatic Cancer Stem Cells
Clinical Implications and Therapeutic Targeting of Cancer Stem Cells (CSCs)
As our knowledge of cancer deepens, it becomes evident that not all tumor cells are alike. Among them, cancer stem cells (CSCs) have emerged as particularly influential due to their unique capabilities. This distinction has several clinical implications and opens up avenues for novel therapeutic interventions.
Monitoring Metastasis-Initiating Cells for Treatment Efficacy
CSCs are believed to be the chief architects of metastasis, the spread of cancer to other parts of the body. Therefore, tracking these metastasis-initiating cells could offer a real-time insight into how well a treatment is working. If therapies are effective, one would expect a reduction in the numbers or activity of these cells. Conversely, an uptick might indicate that the treatment isn't effectively curbing the cancer's aggressive spread, prompting a reconsideration of therapeutic strategies.
Cancer Stem Cells as Prognostic Markers and Indicators of Metastasis Risk
Given their unique attributes, CSCs can serve as a double-edged sword in cancer progression. On one hand, their presence in a tumor may indicate a more aggressive cancer type, given their inherent resistance to traditional therapies and propensity for metastasis. On the other, identifying these cells can offer invaluable insights into patient prognosis. For instance, higher concentrations of CSCs in a tumor might suggest an elevated risk for metastasis, aiding clinicians in tailoring more aggressive and targeted treatments for such patients.
Targeted Therapies: The Way Forward
Given their crucial role, CSCs are ripe targets for innovative therapies. Here's a look into the therapeutic landscape:
Cell Surface Proteins
Certain proteins are present predominantly on the surface of CSCs. Drugs or antibodies targeting these proteins can offer a selective attack, ensuring the destruction of these cells while sparing healthy cells.
Signaling Pathways
CSCs rely on intricate cellular communication channels, or signaling pathways, for survival and proliferation. Interrupting these pathways can curtail their growth. For instance, drugs that block signals which the CSCs depend upon can effectively starve these cells or render them more susceptible to other treatments.
EMT Modulation
The epithelial-to-mesenchymal transition (EMT) is a process that equips cells with invasive traits, often bolstering the CSCs' metastatic capabilities. Targeting molecules and pathways involved in EMT might suppress this transformation, curbing the cells' invasive tendencies.
MicroRNAs (miRNAs)
These are tiny RNA molecules that regulate gene expression. Some miRNAs are implicated in maintaining the stem-like properties of CSCs. By targeting these specific miRNAs, one could potentially disarm the CSCs.
Challenges and the Road Ahead
While the therapeutic potential is promising, there are hurdles. The very adaptability of CSCs means they can evolve resistance to treatments. Furthermore, while some markers are present predominantly on CSCs, they might also be found on healthy cells, raising concerns about potential side effects.
However, as our understanding expands, the hope is to refine these treatments, making them more selective and potent against CSCs. By focusing on these pivotal players in the cancer saga, we might be one step closer to turning the tide in the fight against this formidable disease.
Genetic Testing
Cancer stem cells (CSCs) play a major role in tumor initiation, progression, metastasis, and recurrence after therapy. A core challenge is that CSCs tend to be resistant to conventional cancer treatments like chemotherapy and radiation. They utilize various mechanisms to evade elimination by standard therapies, posing a major obstacle. There is an urgent need for new therapeutic strategies able to selectively target and destroy CSCs.
Natural compounds from botanical sources offer potential advantages in this regard. Many plant-derived compounds exhibit anti-inflammatory, antioxidant, and anticancer properties that could impair critical CSC signaling pathways. Additionally, natural compounds may have safer toxicity profiles than current chemotherapies, enabling chronic dosing. Their multitargeted mechanisms of action could also help overcome treatment resistance issues.
This paper will review key preclinical evidence supporting certain natural substances as promising candidates for selectively targeting CSCs. Compounds like curcumin, resveratrol, epigallocatechin gallate (EGCG), quercetin, and sulforaphane demonstrate preliminary anti-CSC activity in lab models. Their abilities to inhibit EMT, self-renewal, viability, and drug resistance pathways in CSCs highlights their therapeutic potential. While challenges remain in optimizing formulations and dosing, natural compounds may hold unique promise for effectively eliminating dangerous CSCs. Selective anti-CSC agents could revolutionize treatment and prevention of tumor recurrence and metastasis.
Curcumin
Curcumin is a polyphenolic compound derived from the Indian spice turmeric. It has been used medicinally for centuries in Ayurvedic medicine and also as a food additive. Curcumin harbors potent anti-inflammatory, antioxidant, and anticancer properties that make it an attractive candidate for targeting cancer stem cells.
Through its diverse pharmacological effects, curcumin appears capable of modulating numerous molecular pathways involved in maintaining CSCs. Studies indicate it can target key signaling molecules like Wnt, Notch, Hedgehog, STAT3, and NF-kB that are dysregulated in CSCs to promote their self-renewal and survival. This multifaceted targeting could help overcome CSC resistance mechanisms.
Specifically, curcumin has been shown in preclinical models to reduce the expression of CSC markers and the size of the CSC subpopulation in breast, colorectal, pancreatic, and head and neck cancers. It also inhibits spheroid formation and serial passage of CSCs derived from various malignancies. These effects are consistent with impairment of self-renewal, which is the hallmark of CSCs.
Beyond direct anti-CSC activity, curcumin also demonstrates several properties that can synergize with and potentiate other therapies. It can sensitize CSCs to radiation and chemotherapies like paclitaxel and gemcitabine, possibly by suppressing survival signaling and drug efflux mechanisms. Curcumin also alleviates therapy-induced enrichment of the CSC population that often occurs with certain treatments.
Curcumin’s pleiotropic mechanisms targeting CSC signaling, self-renewal, and chemoresistance pathways position it as a promising natural agent against CSCs, both as a standalone therapy or combined adjunct. Further research should continue to explore curcumin’s anti-CSC properties.
Resveratrol
Resveratrol is a natural polyphenol abundant in the skins of grapes, berries, and peanuts. It possesses well-established antioxidant, anti-inflammatory, and anticancer properties. Resveratrol affects multiple signaling pathways relevant to cancer stem cells, including STAT3, Wnt, Notch, and NF-kB among others. This multi-targeted activity makes it an attractive anti-CSC candidate.
Several preclinical studies demonstrate resveratrol’s ability to suppress cancer stem cell propagation and viability across various malignancies. In models of breast, pancreatic, colorectal, and ovarian cancers, resveratrol effectively reduces expression of CSC markers, inhibits spheroid formation, and decreases the CSC subpopulation. These anti-self-renewal effects are likely mediated through resveratrol’s impact on developmental and pro-survival signaling pathways that maintain CSCs.
In addition to direct CSC-targeting activity, resveratrol also shows potential to synergize with and enhance other therapies. Combining resveratrol with paclitaxel, doxorubicin, or radiotherapy demonstrates improved efficacy in eradicating CSCs and preventing enrichment post-treatment compared to single agents. This chemosensitization may result from resveratrol suppressing survival signaling and drug efflux in CSCs.
Resveratrol’s multifaceted ability to attenuate CSC propagation, viability, and treatment resistance makes it an promising anti-CSC agent, both alone or paired with other modalities. Further research should continue exploring resveratrol’s utility against lethal cancer stem cells.
Epigallocatechin Gallate (EGCG)
Epigallocatechin gallate, better known as EGCG, is a highly abundant polyphenol found in green tea. It possesses well-documented antioxidant, anti-inflammatory, and anticancer properties. In the context of targeting cancer stem cells, EGCG has been shown to modulate key pathways involved in CSC maintenance, including Hedgehog, Wnt, Notch, STAT3, and NF-kB signaling.
Studies indicate EGCG can reduce the CSC subpopulation and suppress spheroid formation in breast, colorectal, pancreatic, and nasopharyngeal cancer models. It also decreases expression of CSC surface markers and pluripotency maintaining factors. These anti-CSC effects are thought to result from EGCG’s ability to inhibit self-renewal and survival signaling.
Additionally, EGCG may help tackle the chemotherapy resistance of CSCs. EGCG reverses ABC drug transporter activity in various cancer cell types, which could prevent CSCs from ejecting chemotherapies. It also attenuates pro-survival autophagy in CSCs that enables them to withstand drug-induced stress.
Furthermore, EGCG exhibits synergistic activity when combined with other agents. The pairing of EGCG and vitamin E succinate demonstrates enhanced ability to induce apoptosis and growth inhibition in breast CSCs compared to either compound alone. Such synergism further highlights EGCG’s utility as part of a multi-targeted anti-CSC regimen.
In summary, via modulation of pivotal CSC pathways, overcoming drug resistance, and synergistic interactions, EGCG is a promising natural agent against lethal cancer stem cells worthy of further research.
Quercetin
Quercetin is a naturally occurring flavonoid present in many fruits, vegetables, and teas. It displays pleiotropic pharmacological activities including antioxidant, anti-inflammatory, and epigenetic modulating effects. Quercetin affects numerous signaling pathways dysregulated in cancer stem cells, making it a broad targeting anti-CSC agent.
Studies show quercetin reduces the proportion of breast, gastric, and hepatocellular carcinoma cells expressing CSC markers. It also impairs self-renewal capacity based on decreased mammosphere formation in breast CSCs and reduced serial passage ability of colorectal CSCs. These anti-CSC properties may result from quercetin’s inhibition of STAT3, Notch, Wnt, and other pro-survival signaling.
Quercetin also exhibits activity against epithelial-to-mesenchymal transition (EMT), a process which is associated with acquisition of CSC properties. It suppresses EMT regulators like Snail, Slug, and Twist to prevent induced EMT in breast and ovarian cancer models. This could help block genesis of metastatic stem cells.
Additionally, quercetin shows promise in re-sensitizing resistant CSCs to chemotherapies. Co-treatment with quercetin enhances killing of ovarian spheroid-derived CSCs by cisplatin. It also augments the efficacy of gemcitabine against treatment-refractory pancreatic CSCs. Thus quercetin represents a promising chemosensitizing agent.
Through modulation of CSC signaling, impediment of EMT, and chemosensitization, quercetin exhibits diverse anti-CSC properties that warrant further exploration as both a standalone and adjunctive therapy against malignant stem cells.
Sulforaphane
Sulforaphane is a natural compound derived from cruciferous vegetables like broccoli, cabbage, and kale. It has well-established antioxidant and chemopreventive activity. Sulforaphane acts as a histone deacetylase (HDAC) inhibitor, enabling it to alter gene expression in cancer stem cells to impair their propagation and survival.
Studies have shown sulforaphane selectively targets and eliminates breast cancer stem cells while demonstrating little toxicity to normal mammary stem cells. It reduces secondary mammosphere formation and decreases the ALDH-positive CSC subpopulation. Sulforaphane also showed efficacy against pancreatic CSCs. This selectivity and CSC-directed cytotoxicity highlights its promise.
In addition to direct anti-CSC effects, sulforaphane also re-sensitizes resistant CSCs to chemotherapies. It was found to inhibit drug efflux mediated by ABC transporters in breast CSCs. Combined treatment with sulforaphane and doxorubicin enhanced apoptotic cell death compared to either as monotherapies. Thus, sulforaphane may help reinvigorate the efficacy of standard chemotherapy regimens against otherwise resistant CSCs.
In summary, sulforaphane exhibits dual efficacy against CSCs - directly targeting their viability and self-renewal, while also overcoming their drug resistance. More research on optimal delivery methods and dosing regimens will help advance sulforaphane as a selective anti-CSC agent.
Conclusion
A growing body of preclinical evidence demonstrates that certain natural compounds exhibit promising anti-cancer stem cell activity, either as standalone agents or in combination with other therapies. Polyphenols like curcumin, resveratrol, EGCG, and quercetin display multi-targeted mechanisms that impair CSC signaling, self-renewal, and survival. Isothiocyanates like sulforaphane directly eliminate CSCs while sparing normal stem cells.
Moving forward, further research is still needed to optimize delivery methods and synergistic combinations for maximal anti-CSC efficacy. Combining natural compounds with each other and with chemotherapies or targeted agents may provide a multi-pronged strategy against lethal CSCs. Determining optimal dosing, timing, and regimens warrants continued investigation.
Translation to human studies poses challenges including achieving sufficient bioavailability and selectivity against CSCs over normal cells. Clinical trials are imperative to evaluate anti-CSC activity, pharmacokinetics, and safety in patients. Biomarker development could help assess target engagement and response.
In conclusion, natural compounds represent a promising avenue for eliminating residual CSCs driving recurrence, metastasis, and treatment resistance. Developing selective CSC-targeting agents could revolutionize cancer survivorship and reduce mortality. The research horizon remains bright for discovering and advancing natural therapies able to successfully target these evasive cells and deliver hope to patients worldwide.