The Importance of the Micro-Environment in Cancer
For decades, cancer research and therapy focused almost exclusively on targeting the cancer cell itself. The predominant view framed cancer as a cell-autonomous disease driven solely by internal gene mutations and cellular signaling gone awry within the transformed clone. Therapeutic efforts accordingly aimed at eliminating or correcting malignant cells by directly targeting their disordered genetics and biology.
This cell-centric model, however, neglected a pivotal dimension shaping the behavior of cancer cells: their dynamic interactions with the surrounding microenvironment. Cancer cells reside nested within a complex milieu of adjacent normal cells, extracellular matrix, and molecules that profoundly influence their fate. Far from being autonomous, emerging research reveals cancer cells participate in an intricate biochemical rumba with their surrounding partners that contributes crucially to tumor progression.
This paradigm shift emerged from accumulating evidence that the non-cancerous cells adjoining malignant clones are not passive bystanders. Rather, these diverse stromal cell types, such as fibroblasts, immune cells, blood and lymphatic endothelium, are active participants regulating cancer cell proliferation, survival, invasion, metabolism, and dissemination to distant sites. Cancer cells, in turn, direct remodeling and recruitment of accessory cells needed to construct a self-serving ecosystem.
This reciprocal molecular dialogue drives the continual evolution of malignant cells through genetic and epigenetic modifications responsive to microenvironmental cues. Therapeutic targeting of cancer cells in isolation often fails because it neglects this collaborative interplay. As our awareness expands, therapies now aim to intercept this alliance by better targeting the tumor microenvironment and crosstalk networks. The rest of this paper will delve into the components, mechanisms, and opportunities for therapeutic targeting of the dynamic signaling loop enabling cancer advancement.
Executive Summary
This article discusses a paradigm shift in cancer research, moving from a cell-centric view to recognizing the importance of the tumor microenvironment. This shift acknowledges that cancer is not just about the malignant cells themselves, but also their interactions with surrounding non-cancerous elements.
The tumor microenvironment is described as an ecosystem of non-cancerous cells, signaling molecules, and structural elements that interact with cancer cells. This complex environment plays a crucial role in tumor growth, progression, and metastasis.
Key components of the tumor microenvironment include immune cells (such as T cells, macrophages, and natural killer cells), cancer-associated fibroblasts, blood and lymphatic vessels, and the extracellular matrix. Each of these components interacts with cancer cells in unique ways.
This article emphasizes the reciprocal signaling between cancer cells and their surroundings, driving cancer progression through a dynamic crosstalk. This bidirectional communication allows cancer cells and stromal cells to co-evolve, creating an environment that increasingly favors tumor growth.
It details how cancer cells communicate with and influence their environment through paracrine signaling networks. This involves the release of various growth factors, cytokines, and other signaling molecules that affect nearby cells and tissues.
The recruitment of pro-tumorigenic immune cells by cancer cells is explained, highlighting how the immune system can be co-opted to support tumor growth. This includes the attraction and "re-education" of immune cells to suppress anti-tumor responses and promote cancer progression.
This article describes how cancer cells activate fibroblasts and remodel the extracellular matrix to aid invasion and metastasis. This involves the transformation of normal fibroblasts into cancer-associated fibroblasts (CAFs) that secrete proteins facilitating tumor growth and spread.
Angiogenesis and lymphangiogenesis in the tumor microenvironment are discussed as crucial processes for tumor growth and spread. Cancer cells stimulate the formation of new blood and lymphatic vessels to supply nutrients and provide routes for metastasis.
The concept of metabolic symbiosis between cancer and stromal cells is introduced, explaining how cancer cells establish beneficial metabolic relationships with surrounding cells. This includes the exchange of metabolites and energy sources between different cell types in the tumor.
Various therapeutic approaches targeting the tumor microenvironment are outlined, including immunotherapy (such as checkpoint inhibitors and CAR T-cell therapy), anti-angiogenic therapies, and strategies targeting cancer-associated fibroblasts. These approaches aim to disrupt the supportive environment that tumors create.
This article explores approaches to target the extracellular matrix and collagen, aiming to disrupt the structural support for cancer cells. This includes strategies like using enzymes to break down collagen, antibodies to block ECM proteins, and inhibitors of matrix-remodeling enzymes.
Natural compounds that may help target components of the tumor microenvironment are discussed, including curcumin, resveratrol, EGCG, boswellic acid, honokiol, cryptotanshinone, and carnosol. Each of these compounds is described with its potential mechanisms of action against various aspects of the tumor microenvironment.
This article concludes by emphasizing the potential of these natural compounds in targeting various aspects of the tumor microenvironment, while noting that more research is needed to validate and optimize their effects. It suggests that these compounds could potentially complement existing cancer therapies by modulating the tumor microenvironment.
Introduction to the Tumor Microenvironment
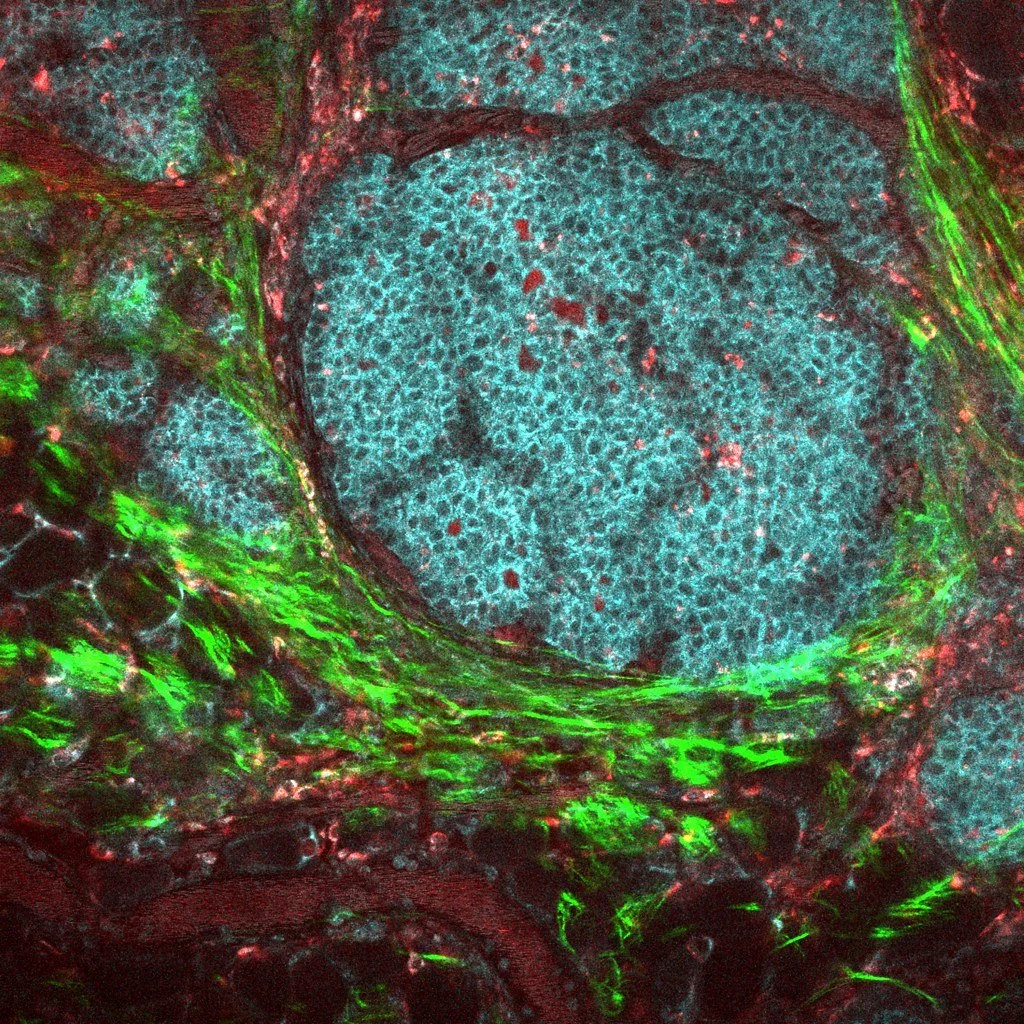
The tumor microenvironment refers to the ecosystem of non-cancerous cells, signaling molecules, and structural elements that surround and intermingle with the cancerous cells in a tumor. Key components of the tumor microenvironment include:
Immune Cells
Diverse immune cell types are drawn to and activated in the tumor microenvironment, including T cells, B cells, natural killer cells, tumor-associated macrophages, myeloid-derived suppressor cells, and more. These immune cells can either suppress or promote tumor growth depending on the balance of cytokines and signaling.
Extracellular Matrix
The non-cellular matrix around tumor cells contains structural proteins like collagen, fibronectin, laminin, and proteoglycans as well as signaling molecules like cytokines, growth factors, hormones, and metabolites.
Cancer-Associated Fibroblasts
Fibroblasts are activated by cancer cell signals to provide structural scaffolding for tumors via extracellular matrix proteins like collagen. Fibroblasts also secrete growth factors supporting angiogenesis and cancer progression.
Blood and Lymphatic Vessels
To fuel their rapid growth, tumors stimulate development of new blood vessels through angiogenesis and lymphangiogenesis. This recruits endothelial cells to construct disorganized, permeable vasculature.
In addition, tissues stressed by malignancy release damage signals called alarmins or DAMPS, including ATP and heat shock proteins, which influence immune responses and tumor-promoting inflammation.
This complex microenvironmental network dynamically evolves along with cancer cells through reciprocal biochemical signaling and cellular recruitment, empowering malignancy. Targeting these collaborative interactions may reveal new treatment approaches.
Reciprocal Signaling Drives Cancer Progression
Far from being an isolated entity, emerging research reveals that a tumor is an ecosystem of malignant cells intricately communicating with surrounding normal cells and structural components. The key thesis is that cancer progression is driven by dynamic crosstalk between cancer cells and diverse elements of the local microenvironment.
Cancer cells continually transmit signals that activate, recruit and reshape the neighboring stroma to construct a supportive habitat catering to their demands. They direct remodeling of the extracellular matrix, stimulate angiogenesis, subvert immune cells, and corrupt normal cell metabolism to fuel their aberrant growth. At the same time, inputs from the microenvironment reciprocally stimulate genetic and epigenetic changes within cancer cells, driving adaptation.
This bidirectional biochemical signaling loop allows cancer cells and collaborative stromal partners to co-evolve in parallel as malignancy progresses. Disrupting this confederacy by intercepting key nodes of microenvironmental crosstalk represents an emerging therapeutic paradigm. Understanding cancer as an ecosystem of co-dependent relationships could reveal promising opportunities to thwart this disease.
Immune Cells in the Tumor Microenvironment
The tumor microenvironment contains a heterogeneous mix of immune cell types, some with tumor-suppressing functions and others that promote growth:
T Cells
CD8+ cytotoxic T cells can mount anti-tumor immune responses. But regulatory T (Treg) cells suppress immunity. The balance controls the outcomes.
Myeloid-Derived Suppressor Cells
Immature myeloid cells expanding during cancer progression inhibit T cell functions and secrete factors that contribute to tumor vascularization and metastasis.
NK Cells
Natural killer cells normally detect and eliminate aberrant cells. But cancer cells can evade NK cell attack via shedding ligands and other tactics.
Dendritic Cells
Normally key antigen presenters, dendritic cells in tumors fail to mature properly and activate T cell responses. Immature dendritic cells contribute to immune tolerance of cancer.
Tumor-Associated Macrophages
Chemicals from cancer cells attract monocytes that differentiate into macrophages. These are subverted to support angiogenesis, matrix remodeling, and immunosuppression.
The complex interplay between the immune system and cancer cells can either stimulate immunity against tumors when properly activated, or be co-opted to shield malignancy from immune attack. Harnessing the body's immune defenses against cancer requires tipping this balance.
Cancer-Associated Fibroblasts (CAFs)
Fibroblasts are activated within tumor microenvironments to become cancer-associated fibroblasts (CAFs). They exert pro-tumorigenic influences through several mechanisms:
CAFs secrete extracellular matrix proteins like collagen and fibronectin that provide physical scaffolding for tumor growth and migration. They also remodel and realign matrix to aid invasion.
CAFs release growth factors including VEGF, FGF, PDGF, HGF, and TGF-beta that support cancer cell survival, proliferation, and metastasis. These paracrine signals propagate through receptors on cancer cells.
CAFs can also directly transfer mitochondria to cancer cells through nanotubes or vesicles. This supplements cancer cell metabolism to provide resistance to therapy.
Through autophagy, CAFs supply cancer cells with recycled nutrients like amino acids, fatty acids, and ketones, fueling growth.
CAFs are mechanically contractile and can influence stiffness of the tumor microenvironment. Stiffness promotes cancer progression.
Overall, CAF activation leads to construction of a tumor matrix scaffold optimally organized to favor cancer cell expansion, sustainment, migration, and metastasis to distant sites. Targeting CAF-cancer cell crosstalk may thereby block these supportive effects.
Endothelial Cells and Tumor Vasculature
To meet their demands for rapid growth and dissemination, cancer cells stimulate formation of new blood vessels in a process called angiogenesis. Lymphangiogenesis also generates draining lymphatic vessels. This recruits endothelial cells that construct the chaotic vasculature permeating tumors:
Angiogenic factors like VEGF and FGF produced by cancer and stromal cells activate quiescent endothelial cells, promoting proliferation and migration to the tumor bed.
Endothelial cells responding to these signals organize into dysmorphic, immature vascular networks displaying abnormal branching, leakiness, and excessive permeability compared to normal vasculature.
Poor perfusion and transit time in this aberrant vasculature creates regional hypoxia and areas of acidosis, driving more angiogenesis and cancer cell adaptation.
The abnormal endothelial-pericyte interactions in newly formed vessels lead to decreased maturity and stability, facilitating cancer cell intravasation into circulation.
Certain endothelial cellscalled tip cells guide new vessel formation using filopodia guided by gradients of VEGF and other factors secreted by cancer cells.
Overall, corrupt angiogenesis and lymphangiogenesis support cancer sustainability and provide highways enabling tumor cells to migrate through circulation to distant tissue sites throughout the body.
Extracellular Matrix Proteins, Cytokines and Growth Factors
In addition to cells, the extracellular milieu around tumor cells contains diverse structural proteins, signaling molecules, and bioactive compounds:
Structural proteins like collagen, laminin, fibronectin, and proteoglycans provide biophysical scaffolding facilitating growth and migration. Matrix metalloproteinases remodeling the ECM also aid invasion.
Growth factors including VEGF, PDGF, HGF, EGF, FGF2, TGFβ promote processes like proliferation, survival, angiogenesis, invasion, and metastasis. Cancers hijack these normally tightly regulated signals.
Inflammatory cytokines such as TNFα, IL-1, IL-6, and IL-8 establish an inflammatory, pro-tumorigenic microenvironment. They recruit immune cells, activate CAFs, and provide survival cues.
Chemokines like CCL2, CXCL12 attract pro-tumorigenic immune cells like tumor-associated macrophages. They also guide organ-specific metastasis.
Metabolites like lactate, secreted by cancer cells through aerobic glycolysis, provide paracrine fuel to cancer cells while suppressing immune activity.
Growth hormone, estrogen, Insulin/IGF-1 and adipokines constitute hormones supporting cancer cell survival and progression.
Therapeutically targeting these extracellular proteins, signals, and metabolites key to cancer-microenvironment interactions may help disrupt the biochemical networks propagating malignancy.
How Cancer Cells Communicate with Their Surroundings
Cancer cells don't act alone - they constantly talk to and influence the normal cells around them through chemical signaling. This allows them to reformat the environment for their own benefit. There's a complex cross-talk network that researchers are trying to understand.
Paracrine Signaling Networks in the Tumor Microenvironment
Paracrine signaling refers to communication between nearby cells via chemical signals secreted into the local environment. This form of signaling enables extensive crosstalk between cancer cells and surrounding stromal cells within the tumor microenvironment:
Cancer cells secrete various growth factors such as VEGF, HGF, EGF, and FGF. These growth factors diffuse locally and bind to specific receptors on nearby endothelial cells, fibroblasts, and immune cells. This stimulates these stromal cells to support processes like angiogenesis, migration, and inflammation.
In response, stromal cells will then release their own signaling molecules like cytokines and chemokines back into the microenvironment. These signals reciprocally act on receptors on cancer cells to influence behaviors like survival, proliferation, invasion, and metastasis.
These paracrine signaling loops create interdependency between the cancer cells and stromal components. This crosstalk helps establish a unique ecosystem optimized for cancer progression.
Signaling interactions between the cancer and stroma increase in complexity over the course of tumor evolution, contributing to cancer heterogeneity and adaptation.
Intricate paracrine signaling networks mediate the dynamic biochemical conversations between cancer cells and the surrounding microenvironment. Targeting and intercepting these conversational biochemical links may represent a promising therapeutic approach.
Cancer Cell Recruitment of Pro-Tumorigenic Immune Cells
Cancer cells have developed clever ways to entice and exploit immune cells that end up promoting rather than combating tumor growth. They accomplish this through several means:
Cancer cells secrete various chemokines and cytokines like CCL2, CSF1, and VEGF into the tumor microenvironment. These chemical signals act as beacons recruiting immune cells like tumor-associated macrophages, myeloid-derived suppressor cells, and regulatory T cells.
Upon recruitment, cancer cells use additional signals like IL-10, TGF-beta, and IDO to activate and "re-educate" the immune cells. This converts them into supporters rather than attackers, often by suppressing cytotoxic activity.
Mechanisms like PD-L1 expression also allow cancer cells to evade detection and subsequent attack by immune cells. This permits immune tolerance of the cancer.
Metabolic dysregulation in cancer cells leads to nutrient starvation and accumulation of metabolic byproducts like lactate that suppress surrounding immune cells.
In this way, populations of immune cells with anti-tumor potential become manipulated by cancer cells into pro-tumor allies. Finding ways to block this immune co-opting or reactivate anti-tumor immunity remains an important therapeutic goal.
Activating Fibroblasts and Remodeling Matrix to Aid Invasion
Cancer cells have co-opted several tricks to get fibroblasts to remodel the surrounding structural matrix in ways that promote tumor invasion:
Cancer cells secrete TGF-beta, PDGF, and other growth factors that act on nearby fibroblasts, stimulating their activation into cancer-associated fibroblasts (CAFs).
CAFs secrete MMPs and other matrix remodeling proteins that break down and reorganize the extracellular matrix surrounding the tumor. This cleaves a path for cancer cells to migrate and invade into local tissue.
CAFs also deposit new matrix proteins like collagen and fibronectin. Alignment and crosslinking of these proteins creates migration "highways" that cancer cells crawl along during invasion.
Contraction of CAFs can increase tissue density and stiffness, further favoring cancer cell motility and metastasis.
Cancer cells have learned to corrupt normal fibroblast function for their own purposes. By co-opting fibroblasts to remodel the structural microenvironment, cancers pave an escape route out of the primary tumor site to infiltrate other tissues. Finding ways to intercept these signals to fibroblasts could have important therapeutic benefits.
Angiogenesis and Lymphangiogenesis in the Tumor Microenvironment
To obtain the nutrients and oxygen necessary to support their rapid growth, cancer cells rely on the process of new blood vessel formation, called angiogenesis. They also stimulate lymphangiogenesis (The formation of lymphatic vessels from pre-existing lymphatic vessels) to generate drainage vessels:
Cancer cells secrete angiogenic growth factors like VEGF that travel locally and bind receptors on nearby endothelial cells, activating them. Activated endothelial cells proliferate, migrate, and organize into new blood vessels penetrating the tumor.
This tumor vasculature is hastily assembled and chaotic, lacking the organization and structural integrity of normal vessels. This allows easier intravasation of cancer cells into circulation.
Lymphangiogenesis induced by cancer cell signaling enables formation of lymphatic capillaries. This unfortunately provides a route for cancer cells to migrate to regional lymph nodes, the first stopping points of metastasis.
Both angiogenesis and lymphangiogenesis are induced not just by cancer cell signals but also by immune cells, fibroblasts, and low oxygen levels in the disordered tumor microenvironment.
Overall, by inducing angiogenesis and lymphangiogenesis, cancers ensure delivery of nutrients to support their growth while also providing highways enabling escape to other body tissues - in essence, building the routes enabling metastasis.
Metabolic Symbiosis Between Cancer and Stromal Cells
Metabolic symbiosis refers to a close, mutually beneficial biochemical relationship between cells involving energy metabolism.
Research shows cancer cells establish metabolic symbiosis with stromal cells in the tumor microenvironment, including fibroblasts, immune cells, and endothelial cells. Some examples include:
Cancer cells increase glycolytic metabolism and lactate production while stromal cells increase oxidative metabolism. The stromal cells take up and metabolize lactate secreted by cancer cells as fuel.
Cancer cells deficient in certain amino acids or nutrients rely on stromal cells to synthesize and provide these metabolites. This supports the bioenergetic demands of cancer cells.
Oxidative stress in cancer cells leads them to depend on stromal cells taking up ROS to help maintain redox balance.
Fibroblasts undergo autophagy and transfer recycled nutrients like amino acids and fatty acids to fuel cancer cell growth.
In summary, metabolic compartmentalization and nutrient exchange establish co-dependency between cancer cells and surrounding stromal cells. This metabolic symbiosis allows cancer cells to partially outsource aspects of their aberrant metabolism to supporting cells in the microenvironment.
Targeting Tumor Angiogenesis
Since developing a blood supply is critical for tumor growth and metastasis, restricting angiogenesis has become an important therapeutic strategy:
VEGF Inhibitors: Antibodies or solubile receptors block VEGF signaling essential for endothelial activation and vessel formation. Examples include bevacizumab, aflibercept, ramucirumab.
Multikinase Inhibitors: Small molecules inhibit multiple kinase enzymes like VEGFR, FGFR, PDGFR that driveangiogenesis signaling. Examples include sunitinib, sorafenib, pazopanib.
Angiopoietin Inhibition: Blocking angiopoietin signaling impairs vessel maturation and stability. Example agents include trebananib.
Coagulants: Damaging existing vasculature by provoking localized clotting and rupturing tumor blood vessels, e.g. with TNF.
Endostatin Therapy: Recombinant endostatin fragments block angiogenesis signaling by binding angiogenic growth factor receptors.
Adhesion Blockade: Inhibiting endothelial cell adhesion molecules like integrins that facilitate vessel growth.
Overall, these approaches aim to regress the supporting tumor vasculature by intercepting signals driving angiogenic activation, vessel growth, maturation, and permeability. Cutting off the blood supply starves tumors of oxygen and nutrients.
Immunotherapy Approaches
Exciting advances have been made in harnessing the immune system to treat cancer by targeting cells in the tumor microenvironment:
Checkpoint Inhibitors: Blocking immune checkpoints like PD-1, PD-L1 and CTLA-4 unleashes and enhances endogenous anti-tumor immunity.
CAR T-cell Therapy: Engineer patient T-cells to express chimeric antigen receptors recognizing cancer cell antigens to better target malignancy.
Cancer Vaccines: Stimulate immune responses against tumor-associated antigens through vaccines that activate cytotoxic T lymphocytes and antibody production.
Oncolytic Virus Therapy: Viruses engineered to selectively infect and damage tumor cells can provoke anti-tumor immunity via release of damage-associated antigens.
Adoptive T cell Transfer: Isolate and expand populations of anti-tumor T cells to actively attack malignancy upon re-infusion into patients.
Dendritic Cell Therapies: Activate patient-derived dendritic cells ex vivo then administer them to initiate robust cytotoxic T cell responses against tumors.
These approaches all work by harnessing and enhancing the patient’s own immune system to recognize and attack cancer. Further refinements and combinations aim to expand the proportion of patients who respond.
Targeting Cancer-Associated Fibroblasts
Since fibroblasts play a major supportive role in the tumor microenvironment, blocking their pro-tumorigenic activation has become a strategy:
Vitamin D: Actives vitamin D compounds inhibit activation of quiescent fibroblasts into cancer-associated fibroblasts. This may involve impeding TGF-beta signaling.
Sonic Hedgehog Inhibitors: The hedgehog pathway is involved in CAF activation and matrix remodeling. Small molecule inhibitors like vismodegib suppress hedgehog signaling.
TGF-beta Inhibition: Blocking TGF-beta signaling may prevent conversion of normal fibroblasts into pro-tumorigenic CAFs. Approaches target TGF-beta production, processing, or receptor binding.
PDGF/FGFR Inhibition: Restricting PDGF and FGF receptor activation on fibroblasts using antibodies or small molecules could block their recruitment and activation by cancer cell signals.
LOX Inhibition: Lysyl oxidase secreted by hypoxic cancer cells stimulates collagen crosslinking by CAFs. LOX inhibitors prevent structural matrix changes favoring invasion.
CAF Depleting Drugs: Selectively inducing apoptosis of CAFs using targeted agents could deplete the supportive fibroblasts in the microenvironment.
Preventing the activation and co-opting of fibroblasts could cutoff a major source of matrix remodeling, growth factors, nutrients, and other supportive mechanisms driving cancer progression.
Targeting the Extracellular Matrix and Collagen
Since remodeling of the extracellular matrix by fibroblasts and proteases enables invasion and metastasis, directly targeting these structural proteins is being explored:
Strategies to Target the Tumor Extracellular Matrix (ECM)
Collagenases - Bacterial collagenase enzymes break down collagen fibers in the ECM. This may dismantle the abnormal rigid scaffolding of fibers that cancer cells rely on to move and spread.
Anti-ECM Antibodies - Antibodies can be designed to bind and block abundant ECM proteins like fibronectin, tenascin-C, and periostin to disrupt organizational assembly of the matrix.
MMP Inhibitors - Matrix metalloproteinases (MMPs) shape the ECM but can also drive tissue breakdown enabling invasion. Inhibitors would block these MMP effects.
Hyaluronidase - This enzyme breaks down hyaluronan, an ECM component influencing tumor interstitial pressure and cell migration. Reducing hyaluronan may help normalize the ECM structure.
FAK/Integrin Inhibitors - Blocking focal adhesion kinase (FAK) and integrins would interfere with cancer cell adhesion to ECM proteins like fibronectin, slowing their migration.
LOX Inhibitors - Lysyl oxidase (LOX) promotes collagen cross-linking to increase ECM rigidity. Inhibitors prevent this stiffening that facilitates invasion.
ECM Digestion - Delivering protease enzyme cocktails to digest ECM components, or using compounds like relaxin to soften the matrix.
Normalization and disruption of the abnormal tumor ECM seeks to revert microenvironmental changes that cancer cells rely on for sustenance and movement.
Natural compounds that may help target components of the tumor microenvironment
Curcumin
Curcumin is a polyphenol from the turmeric spice. It has shown ability to improve efficacy of PD-1/PD-L1 checkpoint inhibitor immunotherapy in preclinical studies. Mechanisms may involve stimulating cytotoxic T cell activity and decreasing regulatory T cells and MDSCs.
Curcumin also demonstrates anti-angiogenic effects by inhibiting growth factors like VEGF and reducing endothelial cell proliferation and migration. This restricts tumor vascularization.
Boswellic Acid
Boswellic acid, from the frankincense herb, can inhibit LOX enzymes which enable collagen crosslinking in the tumor ECM. This prevents stiffening to block invasion.
Reported anti-angiogenic effects may also restrict the tumor blood supply by inhibiting growth factors.
Carnosol
Carnosol is a natural phenolic diterpene found in rosemary.
It has demonstrated ability to inhibit activation of fibroblasts into pro-tumorigenic cancer-associated fibroblasts (CAFs) in lab studies using lung and breast cancer cell models.
Carnosol also possesses anti-angiogenic and anti-inflammatory properties that may help normalize the tumor microenvironment.
Resveratrol
Resveratrol, a polyphenol found in grapes and berries, can augment natural killer cell cytotoxicity against tumor cells in lab studies. It also enhances proliferation and function of anti-tumor CD8+ T cells.
Resveratrol exhibits immunomodulatory effects by altering cytokine profiles and reducing accumulation of tumor-promoting immune cells including MDSCs, macrophages, and regulatory T cells.
It also shows anti-angiogenic activity by downregulating VEGF, MMPs, and other pro-angiogenic mediators. This restricts tumor blood vessel growth.
Honokiol
Honokiol is a bioactive compound extracted from magnolia bark. Preclinical studies indicate it can potently suppress tumor angiogenesis by impairing key steps like endothelial cell migration, adhesion, and tube formation.
It inhibits angiogenesis by downregulating angiogenic factors including VEGF, MMPs, and endothelial nitric oxide. Honokiol also demonstrates broad anti-inflammatory effects.
Honokiol has shown anti-proliferative and pro-apoptotic effects on endothelial cells, restricting growth of new tumor blood vessels.
EGCG
The green tea catechin EGCG can promote tumor antigen presentation and sensitize cancer cells to immune attack and cytolysis. It may also counteract immunosuppressive cells like MDSCs and Tregs.
EGCG reduces tumor angiogenesis by inhibiting endothelial cell proliferation, migration, and tube formation. It may suppress VEGF, MMPs, and other angiogenic enablers.
Through MMP inhibition, EGCG can also stabilize the ECM to counteract invasive remodeling.
Cryptotanshinone
Cryptotanshinone is a compound isolated from dandelion root (Taraxacum officinale).
In vitro and animal studies indicate it can inhibit tumor-associated macrophages, a pro-tumorigenic immune cell population. It reduces macrophage recruitment and polarization.
Cryptotanshinone also exhibits potential anti-angiogenic activity by suppressing VEGF and endothelial cell functions to limit tumor vascularization.
Overall, there are promising signals that certain natural compounds may help target immunosuppression, angiogenesis, fibroblasts, ECM remodeling, and other elements of the pro-tumorigenic microenvironment. More research is still needed to validate and optimize these effects.
https://www.mdanderson.org/cancerwise/what-is-the-tumor-microenvironment-3-things-to-know.h00-159460056.html# https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3689267/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9030088/ https://www.mdpi.com/2072-6694/13/9/2053 https://www.aacr.org/about-the-aacr/newsroom/aacr-meeting-news/how-the-tumor-microenvironment-supports-or-stifles-cancer-growth/ https://www.bms.com/media/media-library/scientific-media-resources/exploring-the-tumor-microenvironment.html