Metabolic Theory of Cancer
What if we’ve been missing a major piece of the cancer puzzle? For decades, research has focused on genetic mutations as the drivers of cancer. But emerging science suggests abnormal metabolism is equally important - an idea called the metabolic theory of cancer. This fascinating perspective proposes that it’s not just mutations, but also metabolic dysfunction that allows cancer cells to go rogue.
Metabolic abnormalities provide the fuel and flexibility for rapid growth, while also creating an environment perfect for invasion and metastasis. The evidence linking obesity, inflammation, and other diet and lifestyle factors to cancer risk provides additional support that metabolism matters. This theory opens promising new avenues to starve cancer by targeting its altered metabolism. Join us on a tour of the metabolic underworld of cancer, where we’ll unravel how tumors rewire their appetite for nutrients and how this metabolic trickery might lead to new therapeutic opportunities. It’s time to bring cancer’s forgotten metabolic secrets to light!
Cancer represents a diverse array of diseases united by several key hallmarks - uncontrolled proliferative growth, invasion into surrounding tissues, and metastasis to distant sites. Decades of research have aimed to unravel the molecular underpinnings of cancer development and progression. While genetic mutations in oncogenes, tumor suppressors, and stability genes are clearly major contributors, mutations alone do not fully explain every aspect of tumor pathogenesis.
This has led some researchers to propose an alternative perspective - that dysfunctional energy metabolism is an equally important driver of malignancy. This metabolic theory of cancer posits that abnormalities in how cells process nutrients like glucose and glutamine can produce the phenotypes of uncontrolled growth, local tissue invasion, and metastasis. Proponents argue that targeting cancer metabolism may provide new therapeutic opportunities compared to solely focusing on genomic aberrations.
This paper will review the scientific evidence supporting key tenets of the metabolic theory of cancer. Cancer cells become heavily dependent on glycolysis as their energy source rather than the more efficient mitochondrial oxidative phosphorylation. This aberrant metabolism arises early in cancer development and produces intermediates that fuel uncontrolled proliferation. Metabolic dysregulation also creates a hostile microenvironment facilitating local invasion and metastasis. Furthermore, associations between diet, obesity, inflammation, and cancer risk reinforce metabolic links. These diverse lines of evidence indicate that deranged cellular metabolism is likely a core enabler of carcinogenesis on par with genomic instability. Therapeutically targeting these metabolic dependencies may offer new hope for cancer treatment and prevention.
Executive Summary
Traditional cancer research has focused on genetic mutations as the main cause of cancer. However, recent studies suggest that abnormal metabolism is just as important. This perspective, called the metabolic theory of cancer, proposes that cancer cells grow uncontrollably not just because of genetic changes but also due to how they process energy.
Understanding the metabolic theory of cancer matters because it offers new treatment options by targeting cancer metabolism, which can complement traditional therapies, improve prognosis, empower informed dietary and lifestyle choices, and provide hope for overcoming resistant cancers.
According to this theory, metabolic dysfunction, particularly in mitochondria, can initiate and drive cancer progression. This challenges the traditional view that genetic mutations are the sole primary cause of cancer.
The Warburg effect, where cancer cells rely heavily on glycolysis even in the presence of oxygen, is not just an adaptation but a key mechanism driving cancer growth and potentially causing genetic instability.
The Warburg effect is a fundamental change in how cancer cells produce energy. Normal cells primarily use oxygen to break down glucose for energy in a process called oxidative phosphorylation, which occurs in the mitochondria (the cell's power plants). This is efficient but relatively slow.
In contrast, cancer cells shift to a less efficient but faster process called glycolysis, even when oxygen is available. Glycolysis is a way of breaking down glucose without using oxygen, occurring in the cell's main body rather than in mitochondria. It's like the difference between a slow-burning, efficient fire (normal cells) and a quick, intense blaze (cancer cells).
This shift to glycolysis, despite being less efficient, provides cancer cells with rapid energy and the building blocks they need for fast growth. It's like the cells are trading efficiency for speed, allowing them to outcompete normal cells and grow uncontrollably.
The Warburg effect, named after Otto Warburg who observed it in the 1920s, is now recognized as a hallmark of most cancers. Understanding this metabolic shift is crucial to the metabolic theory of cancer and opens up new possibilities for detecting and treating cancer by targeting its unique energy production process.
This metabolic shift provides cancer cells with the building blocks for rapid growth and creates an environment conducive to invasion and metastasis. It's not just a side effect, but a central feature of cancer biology.
The theory is supported by strong links between cancer risk and metabolic factors such as obesity, inflammation, and diet. These connections suggest that metabolism plays a crucial role in cancer development.
Emerging evidence shows that metabolic abnormalities often precede genetic mutations in cancer development. This timing suggests that targeting metabolism could be key to preventing cancer or catching it very early.
The altered metabolism of cancer cells creates specific vulnerabilities that can be targeted therapeutically. This approach is already being used by some healthcare professionals as a significant part of cancer treatment.
Potential therapies based on this theory include ketogenic diets, fasting regimens, and drugs that target specific metabolic pathways. These are not just future possibilities but current strategies being implemented in cancer care.
This theory explains why many known cancer risk factors (like obesity and chronic inflammation) increase cancer risk, providing a unifying framework for understanding cancer development.
The metabolic approach to cancer treatment aims to "starve" cancer cells by restricting their preferred fuels or disrupting their unique metabolic processes. This strategy is showing promise in clinical applications.
Natural compounds that affect cellular metabolism, such as curcumin and resveratrol, are being studied not just as future possibilities but as current complementary approaches in cancer care.
The metabolic theory doesn't replace the genetic theory of cancer but integrates with it, providing a more comprehensive understanding of cancer biology. Both metabolic and genetic factors are seen as crucial in cancer development and progression.
The metabolic theory of cancer represents a paradigm shift in oncology, offering new hope for more effective, less toxic cancer treatments and prevention strategies. It's not just a promising area of research, but an approach that's already informing cancer care.
Metabolic Theory of Cancer in Depth
What if we’ve been missing a major piece of the cancer puzzle? For decades, research has focused on genetic mutations as the drivers of cancer. But emerging science suggests abnormal metabolism is equally important - an idea called the metabolic theory of cancer. This fascinating perspective proposes that it’s not just mutations, but also metabolic dysfunction that allows cancer cells to go rogue.
Metabolic abnormalities provide the fuel and flexibility for rapid growth, while also creating an environment perfect for invasion and metastasis. The evidence linking obesity, inflammation, and other diet and lifestyle factors to cancer risk provides additional support that metabolism matters. This theory opens promising new avenues to starve cancer by targeting its altered metabolism. Join us on a tour of the metabolic underworld of cancer, where we’ll unravel how tumors rewire their appetite for nutrients and how this metabolic trickery might lead to new therapeutic opportunities. It’s time to bring cancer’s forgotten metabolic secrets to light!
Cancer represents a diverse array of diseases united by several key hallmarks - uncontrolled proliferative growth, invasion into surrounding tissues, and metastasis to distant sites. Decades of research have aimed to unravel the molecular underpinnings of cancer development and progression. While genetic mutations in oncogenes, tumor suppressors, and stability genes are clearly major contributors, mutations alone do not fully explain every aspect of tumor pathogenesis.
This has led some researchers to propose an alternative perspective - that dysfunctional energy metabolism is an equally important driver of malignancy. This metabolic theory of cancer posits that abnormalities in how cells process nutrients like glucose and glutamine can produce the phenotypes of uncontrolled growth, local tissue invasion, and metastasis. Proponents argue that targeting cancer metabolism may provide new therapeutic opportunities compared to solely focusing on genomic aberrations.
This paper will review the scientific evidence supporting key tenets of the metabolic theory of cancer. Cancer cells become heavily dependent on glycolysis as their energy source rather than the more efficient mitochondrial oxidative phosphorylation. This aberrant metabolism arises early in cancer development and produces intermediates that fuel uncontrolled proliferation. Metabolic dysregulation also creates a hostile microenvironment facilitating local invasion and metastasis. Furthermore, associations between diet, obesity, inflammation, and cancer risk reinforce metabolic links. These diverse lines of evidence indicate that deranged cellular metabolism is likely a core enabler of carcinogenesis on par with genomic instability. Therapeutically targeting these metabolic dependencies may offer new hope for cancer treatment and prevention.
A Brief History of the Metabolic Theory of Cancer
The origins of the metabolic theory of cancer can be traced back to the pioneering work of Otto Warburg in the early 20th century. Warburg made the seminal observation in 1924 that cancer cells tend to rely on glycolysis for energy production even in the presence of adequate oxygen. This differed from normal cells that preferentially generate ATP through mitochondrial oxidative phosphorylation. Warburg won the Nobel Prize for his work.
Warburg hypothesized that this aberrant cancer cell metabolism, now known as the “Warburg effect”, was causally linked to malignant transformation. He theorized that irreversible damage to cellular respiration somehow triggers compensatory increases in fermentative glycolysis. However, his broader theory was largely overshadowed and forgotten when the somatic mutation theory rose to prominence in the mid-1900s.
Interest in the metabolic basis of cancer was rekindled in the 1990s and 2000s with additional findings about mitochondrial defects and proliferative metabolism in cancer. Researchers like Peter Pedersen and Matthew Vander Heiden helped reframe the Warburg effect as an optimized adaptation to support biosynthesis, rather than just a consequence of damaged respiration.
In 2011, scientists Thomas Seyfried and Doug Wallace published a landmark paper formally outlining the metabolic theory of cancer. They hypothesized that mitochondrial dysfunction is the prime origin of cancer, with mutations arising later. They argued that impaired mitochondrial function drives compensatory fermentation. This 2006 paper catalyzed renewed interest in cancer metabolism.
While aspects remain controversial, the metabolic theory has gained support from findings on metabolic abnormalities predating mutations, metabolite-driven epigenetics, links between obesity/diabetes and cancer, and preliminary successes of metabolic-based therapies. Ongoing research aims to further evaluate if bioenergetic dysregulation is causal or just correlational in cancer development and progression.
Metabolic Theory of Cancer as an Alternative Perspective
For decades, the dominant model for understanding cancer has centered around genetic mutations and genomic instability as the prime drivers of tumor formation and progression. However, some researchers have recently proposed an alternative paradigm – the metabolic theory of cancer. This theory posits that profound alterations in cellular energy metabolism are equally critical contributors to the malignant phenotypes of uncontrolled proliferation, local tissue invasion, and metastasis.
Proponents of the metabolic theory argue that in addition to mutations, aberrant metabolism of nutrients like glucose, glutamine and fatty acids fundamentally underpin the origins and progression of cancer. These metabolic abnormalities arise early, often even before genomic instability occurs, and produce the biosynthetic intermediates that fuel rapid growth. Metabolic dysfunction also creates an abnormal microenvironment facilitating invasion and metastasis. The metabolic theory thus presents a shift in perspective from only targeting genetic mutations to also targeting cancer metabolism as a key antineoplastic approach.
This paper will review the scientific evidence supporting several core tenets of the metabolic theory of cancer. First, it will discuss how cancer cells acquire altered metabolism optimized for proliferation rather than efficient ATP production. Second, it will examine how these metabolic derangements enable cancer phenotypes and behaviors on a functional level. Third, it will highlight links between diet, clinical risk factors like obesity and inflammation, and cancer outcomes as further evidence for metabolic underpinnings. Finally, it will explore emerging therapeutic strategies to target cancer metabolism. Overall, the diverse supportive evidence argues that an altered metabolic program is equally as important as genomic instability to the pathogenesis and progression of cancer.
Aberrant Energy Metabolism Drives Malignancy
While genetic mutations have long been considered the predominant force behind cancer, an alternative perspective called the metabolic theory of cancer has emerged to challenge this view. This theory proposes that alongside mutations, profound derangements in cellular energy metabolism are equally critical drivers of malignant transformation and cancer progression.
According to the metabolic theory, abnormalities in how cells metabolize and utilize nutrients like glucose, glutamine, and fatty acids fundamentally enable the hallmark phenotypes of cancer - uncontrolled proliferation, invasion, and metastasis. These metabolic dysfunctions arise early in cancer development and are not just byproducts of malignant transformation. Instead they actively generate the necessary building blocks and supportive microenvironmental conditions that allow cancer cells to thrive.
The key thesis underpinning the metabolic theory is that aberrant energy metabolism itself represents a core mechanism directly promoting the initiation and progression of cancer, not just a consequence of it. Thus targeting deregulated metabolic pathways could provide novel antineoplastic strategies on par with targeting genomic mutations. This reframing challenges the traditional somatic mutation-centric view of cancer biology.
This paper will synthesize the diverse strands of evidence supporting the vital role of metabolic abnormalities in the development and progression of cancer. First it will outline the major metabolic rearrangements in cancer cells. Next it will elucidate how these derangements functionally enable malignancy through effects on proliferation, invasion, microenvironment, and more. Finally, it will highlight connections with clinical risk factors as further evidence for metabolic underpinnings of carcinogenesis. This multifaceted supportive evidence substantiates bioenergetic dysfunction as a primary driver of cancer, rather than just a passive participant.
Shift to Glycolysis - The Warburg Effect
One of the most well-established metabolic alterations in cancer cells is increased dependence on glycolysis as their primary energy source, rather than the more efficient mitochondrial oxidative phosphorylation (OXPHOS). This phenomenon is known as the Warburg effect or aerobic glycolysis, and was first observed by Otto Warburg in the 1920s.
Normal differentiated cells rely heavily on OXPHOS to generate ATP, using glucose, fatty acids and glutamine as primary fuels. OXPHOS couples nutrient oxidation to ATP synthesis via the electron transport chain and ATP synthase complex. In contrast, cancer cells display reduced OXPHOS activity and increased glycolysis, converting most incoming glucose directly to lactate. This persists even in oxygen-rich conditions, hence the term “aerobic” glycolysis.
While much less efficient for ATP production on a per molecule basis, glycolysis provides several advantages to cancer cells. It generates metabolic intermediates like ribose, glycerol, citrate and NADPH that are indispensable for rapid proliferation. It also reduces dependence on mitochondria, which produce damaging reactive oxygen species. Thus this metabolic shift empowers the unrestrained growth that is the hallmark of cancer.
The Warburg effect is now recognized as a near universal feature of most tumors. While the exact mechanisms triggering increased glycolysis remain incompletely understood, major factors likely include hypoxia, oncogenic signaling, and mitochondrial defects - all of which can upregulate glycolytic enzymes and transporters while down regulating OXPHOS. Targeting this shift to glycolysis is a promising therapeutic approach.
Mechanisms Leading to Increased Glycolysis
While the Warburg effect is widely recognized in cancer, ongoing research continues investigating precisely how cancer cells make the metabolic shift to glycolysis. Several key molecular mechanisms have been identified:
HIF-1α Activation
The transcription factor HIF-1α is a master regulator of cellular responses to low oxygen. HIF-1α activates the expression of multiple glycolytic enzymes and transporters to promote anaerobic glycolysis for ATP production. It also suppresses mitochondrial respiration by inhibiting pyruvate dehydrogenase. Even in the absence of hypoxia, oncogenic signaling and loss of tumor suppressors leads to increased HIF-1α, driving the Warburg effect.
Oncogenic Signaling
Hyperactivation of growth-promoting oncogenes likewise propels metabolic reprogramming towards glycolysis. Myc upregulates glycolytic genes and supports mitochondrial biogenesis. Ras promotes glucose uptake and channeling into glycolytic versus mitochondrial pathways. Akt activates aerobic glycolysis by increasing expression and membrane localization of glucose transporters and glycolytic enzymes.
In summary, increased glycolytic metabolism in cancer arises from complex interplay between oxygen sensing pathways, oncogenic signals that amplify nutrient uptake and metabolism, and loss of tumor suppressors that impose metabolic constraints. Targeting glycolysis requires an understanding of these diverse drivers.
Loss of p53 Function
The tumor suppressor p53 inhibits glycolysis and enhances mitochondrial respiration via effects on gene expression and protein interactions. Hence, p53 inactivation in cancer cells contributes to the Warburg effect by releasing the brakes on glycolysis. This may help explain the prominence of aerobic glycolysis in cancers where p53 is mutated.
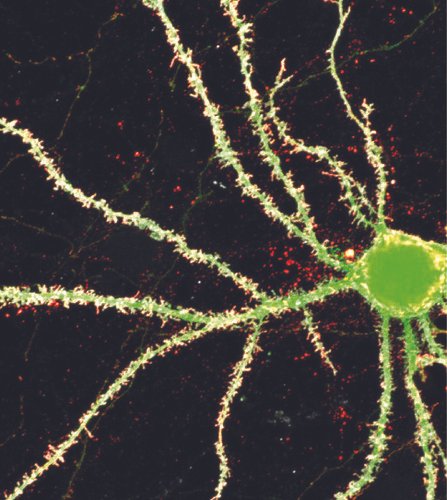
Impaired Mitochondrial Function and Increased ROS
While cancer cells become heavily reliant on glycolysis, mitochondrial function is also profoundly altered in malignancy. Cancer cell mitochondria exhibit several abnormalities:
Impaired Respiration - Components of the electron transport chain complexes show reduced expression and activity, compromising oxidative phosphorylation capacity.
Increased ROS - Damaged or defective mitochondria in cancer cells produce excessive reactive oxygen species (ROS). High ROS can cause further mitochondrial dysfunction.
Altered Structure - Cancer cell mitochondria manifest structural changes like abnormal cristae, indicative of compromised function. Mutations in mtDNA undermine integrity.
Imbalanced Dynamics - Mitochondrial biogenesis, fission/fusion, mitophagy and motility processes are dysregulated, further disrupting normal mitochondrial physiology.
These mitochondrial defects are thought to be partly responsible for the shift to glycolysis. However, mitochondria are not completely inert - cancer cells leverage mitochondrial metabolism for key biosynthesis intermediates and redox regulation. This mitochondrial reprogramming is facilitated by changes in gene expression patterns driven by oncogenic signals and loss of tumor suppressors.
The high ROS output from dysfunctional cancer mitochondria also has important implications. Elevated ROS triggers oxidative damage to DNA, proteins, and lipids, fostering genomic instability. ROS also activates pathways that promote proliferation, survival, and metastasis. Thus mitigating oxidative stress is likely an important adaptation in cancer’s altered metabolism.
In summary, cancer cells undergo remodeling of mitochondrial networks and utilization to support malignant phenotypes, despite impaired respiratory capacity. Aberrant mitochondrial function is both a driver and consequence of metabolic rearrangements in cancer.
Enhanced Glutaminolysis and Glutathione Dependence
In addition to increased glycolytic metabolism of glucose, cancer cells also display altered utilization of other key nutrients, notably glutamine. Glutamine metabolism undergoes major upregulation to fuel biosynthesis and cellular defense pathways.
Glutaminolysis, the breakdown of glutamine to lactate, is markedly enhanced in many cancers to provide intermediates that feed the tricarboxylic acid (TCA) cycle and lipid production. Glutamine also provides nitrogen for synthesis of nucleotides and amino acids. The increased dependence on glutaminolysis results from oncogenic signals like Myc that induce glutamine transporters and catabolic enzymes.
Cancer cells also divert glutamine into the glutathione biosynthesis pathway. Glutathione is the major antioxidant that neutralizes ROS. The heightened ROS output in cancer cells drives demand for glutathione. Glutamine feeds this pathway by providing glutamate and cysteine precursors. This glutathione dependence makes cancer cells more vulnerable to glutamine restriction.
Cancer cells enhance both glutaminolysis and glutathione production from glutamine to meet biosynthetic and antioxidant needs. Targeting these key nodes of glutamine metabolism and dependency represents a promising therapeutic avenue. Ongoing research aims to fully understand the rewiring of glutamine metabolism in cancer.
Nutrient Deficiencies in Cancer Cells
The altered metabolic program in cancer cells, while optimized for rapid proliferation, also creates paradoxical deficiencies in certain nutrients. Two key nutrient deficiencies resulting from the abnormal metabolism of cancer cells include:
Glucose Deprivation Despite increased glucose uptake and glycolytic metabolism, cancer cells can experience intracellular glucose deprivation. This results because the majority of imported glucose is diverted into biomass production pathways like the pentose phosphate shunt rather than made available for energy metabolism. This glucose deprivation creates metabolic stress to which cancer cells adapt via signaling pathways.
Essential Amino Acid Deficiencies Cancer cells require higher amounts of non-essential amino acids like glutamine and aspartate to match their rapid anabolism. However, they are unable to sufficiently synthesize essential amino acids needed for protein synthesis. This leads to deficiencies in essential amino acids like methionine that must be imported. Transporters for essential amino acids are thus often upregulated in cancer.
These nutrient deficiencies force cancer cells to radically upregulate intake of carbon and nitrogen sources like glucose, glutamine and essential amino acids. However, this high intake rate is often unsustainable, resulting in microenvironmental depletion of nutrients. This metabolic competition creates an additional selective pressure favoring more aggressive cancer cell clones capable of enhanced nutrient capture.
The altered metabolic priorities of cancer cells tend to create deficits in key nutrients they require in high amounts. This drives compensatory nutrient acquisition mechanisms as well as selection for more metabolically competitive phenotypes.
The nutrient deficiencies created by the abnormal metabolism of cancer cells are important for several reasons:
They represent a metabolic vulnerability that could potentially be exploited therapeutically. Strategies to exacerbate nutrient deficiencies specifically in cancer cells could induce selective metabolic catastrophe.
The deficiencies drive compensatory mechanisms like increased nutrient transporter expression. These mechanisms could be therapeutic targets to cut off the heightened nutrient supply that cancer cells require.
Competition between tumor cells and normal cells for scarce nutrients in the microenvironment generates selective evolutionary pressures. Cells capable of enhanced nutrient capture outcompete other cells, leading to dominance of more aggressive clones. Understanding this process has implications for tackling tumor heterogeneity and adaptation.
Therapies that target specific metabolic pathways may inadvertently aggravate existing nutrient deficiencies in cancer cells or create new ones. These potential deficiency states need to be studied to optimize treatment strategies and avoid resistance.
In summary, the nutrient deficiencies created by the abnormal metabolic priorities of cancer cells significantly impact the evolution of tumors, their responses to therapies, and opportunities for targeted metabolic intervention. Appreciating why these deficiencies occur and how cancer cells compensate is key to advancing cancer metabolism knowledge and treatment.
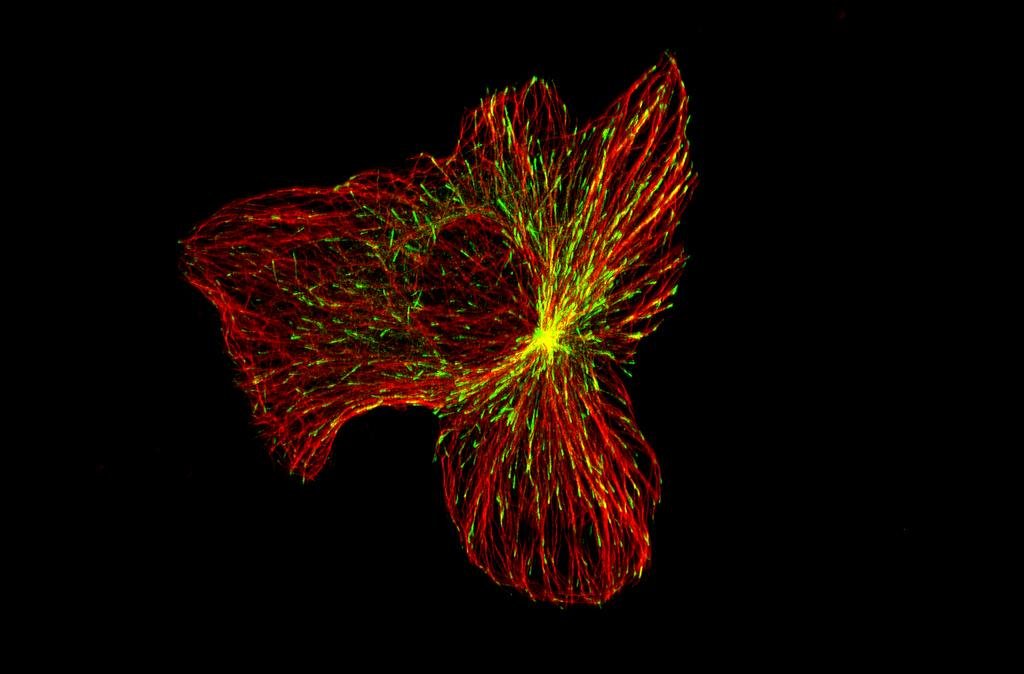
Metabolic Derangements Empower Cancer Growth
Cancer’s altered metabolism provides more than just ATP - it equips cells with the necessary building blocks and adaptive mechanisms to drive malignancy through the following pathways:
To fuel rapid proliferation, cancer cells increase uptake of glucose and diversion into anabolic subsidiary pathways providing nucleotides, lipids, amino acids, and other critical biomass constituents.
Increased secreted lactate leads to acidification of the tumor microenvironment, which promotes degradation of adjacent normal tissue architecture to facilitate invasion. Lactate also helps cancer cells fuel angiogenesis and metastasis.
Dysfunctional cancer cell mitochondria leak excessive reactive oxygen species which directly damage DNA through mutations and strand breaks, leading to the genetic instability that accelerates cancer progression.
Metabolic intermediates like fumarate and succinate alter epigenetic regulation of gene expression by inhibiting enzymes that modify DNA and histones. This results in aberrant epigenetic landscapes favoring cancer-promoting gene programs.
Cancer cells enhance both glutaminolysis and glutathione antioxidant production to satisfy their biosynthetic and redox defense needs, generating metabolic dependencies.
In summary, while providing ATP, the altered metabolism of cancer cells also furnishes the substrates, adaptive aids, and epigenetic reprogramming necessary to acquire the hallmark traits of uncontrolled proliferation, invasion, survival under stress, angiogenesis, and genomic instability. Targeting these key nodes of dysregulated metabolism may reveal promising new treatment vulnerabilities.
Excess Blood Glucose Promotes Glycolytic Phenotypes
Diets high in simple carbohydrates and calories can produce elevated blood glucose levels. This fuels increased glucose uptake and glycolytic metabolism in premalignant and cancer cells, promoting the Warburg effect. Constant abundance of glucose may select for clones optimally equipped for glycolysis. Dietary restriction lowers blood glucose, slowing cancer growth.
Adipokines and Inflammation Shift Metabolism
Adipose tissue secretes inflammatory cytokines like IL-6 and adipokines including leptin. These factors induce signaling associated with insulin resistance, glycolysis, lipogenesis and angiogenesis - pathways hijacked in cancer cells. Chronic inflammation also damages mitochondria. This metabolic reprogramming driven by inflammation and adipokines promotes malignancy.
Oxidative Stress Alters the Microenvironment
Obesity is associated with systemic oxidative stress and reactive oxygen species generation, contributing to genetic mutations. ROS and inflammatory mediators alsohelp remodel the extracellular matrix and activate signaling pathways that cancer cells co-opt for growth, survival and metastasis. This altered microenvironment facilitates malignancy. ROS can induce DNA damage, which may lead to mutations that drive cancer development. Furthermore, the impact of ROS and inflammatory mediators on the tumor microenvironment, aiding in cancer cell survival and metastasis, is a topic of active research.
In summary, clinical correlations between obesity, diet, inflammation and cancer risk support the metabolic theory of cancer. The circulating factors and altered systemic metabolism associated with these conditions provide a fertile environment for malignancy and likely help shape cancer cell metabolism.
Obesity, Hormones and Growth Factors
Obesity is linked to higher levels of insulin, IGF-1, estrogen and altered adipokines that fuel proliferation and metabolism in cancer cells. Insulin resistance leads to hyperinsulinemia that further promotes mitogenic signaling. The metabolic milieu associated with obesity provides favorable conditions for cancer cell growth.
Therapeutic Targeting of Cancer Metabolism
Targeting Rate-Limiting Enzymes or Transporters
Drugs targeting glycolytic enzymes like hexokinase, lactate dehydrogenase (LDH) and transporters like glucose transporters (GLUTs) aim to restrict the fuel supply powering malignancy. Inhibiting glutamine using transport blockers or synthetic lethality approaches exploits glutamine addictions. Limiting nutrient availability weakens cancer cells.
Metformin and Other Biguanides
These widely used diabetes drugs lower circulating glucose and insulin levels. Preclinical and epidemiological data indicate metformin may also have anti-cancer properties by impairing mitochondrial function and glucose metabolism in cancer cells. Ongoing trials are exploring metformin’s potential as an add-on therapy.
Molecular Testing
Low carbohydrate, high fat ketogenic diets elevate ketones as an alternate fuel source to glucose. This may preferentially starve certain cancers. Caloric restriction also limits circulating fuels. Trials of ketogenic diets and fasting regimes aim to take advantage of differential metabolism between normal and cancer cells.
Fasting
Short fasts trigger metabolic adaptations like decreased glucose and IGF-1 that may selectively protect normal cells while sensitizing cancers. Fasting cycles may enhance chemotherapy tolerability. Ongoing research is optimizing fasting protocols for improved cancer treatment outcomes.
Combination Strategies
Metabolic interventions may synergize with chemotherapy, radiation, and targeted drugs that rely on intact mitochondrial function, reactive oxygen signaling, or nutrient availability. Adaptive resistance pathways blocked by drugs may be circumvented by simultaneously restricting key metabolites. Optimizing combinations is a key goal.
In summary, therapeutic targeting of cancer metabolism is an emergent field building on decades of basic research into metabolic abnormalities in cancer. While challenges exist, restricting cancer’s metabolic flexibility may unlock new treatment strategies and sensitize tumors to other modalities.
Natural substances that may help target cancer cell metabolism based on preliminary research:
Curcumin
This polyphenol found in turmeric can inhibit glycolysis, suppress growth signaling pathways like PI3K/Akt/mTOR that drive metabolic reprogramming, and increase ROS generation in cancer cells.
Berberine
This plant alkaloid found in herbs like goldenseal may inhibit glycolysis, mitochondrial function, and glutamine metabolism in cancer cells.
Omega-3 Fatty Acids
Fish oil fatty acids DHA and EPA can increase oxidative stress, lipid peroxidation, and mitochondrial damage in cancer cells.
Resveratrol
This antioxidant compound from grapes can inhibit aerobic glycolysis, decrease GLUT transporters, and sensitize cancer cells to metformin.
Quercetin
This flavonoid in fruits and veggies can reduce glycolytic gene expression, decrease ATP production, and downregulate growth signaling pathways.
EGCG
The green tea catechin EGCG can reduce glucose uptake, inhibit glycolytic enzymes, decrease growth signaling, and re-sensitize cancer cells to chemotherapy.
Tetrathiomolybdate
A copper chelator derived from vegetables that can suppress angiogenesis by inhibiting hypoxia signaling. May starve tumors by pruning blood vessels.
While research is still early-stage, these and other natural compounds show potential to target cancer cell metabolism through diverse mechanisms including inhibiting glycolysis, reducing glucose uptake, increasing oxidative stress, disrupting energy metabolism, and more. Their multi-modal actions make them promising candidates for further exploration.
Conclusion
In summary, a review of the scientific evidence demonstrates that cancer cells undergo a metabolic shift resulting in increased dependence on glycolysis, enhanced glutaminolysis and glutathione pathways, and dynamic nutrient uptake to support malignant proliferation. These metabolic derangements arise early in tumorigenesis and actively contribute to cancer phenotypes rather than passively resulting from them.
Correlations between circulating fuels, obesity, inflammation and cancer development provide further clinical evidence for metabolic underpinnings of malignancy. While the somatic mutation theory has dominated for decades, the metabolic theory argues that mitochondrial dysfunction and ensuing compensatory metabolic reprogramming are equally important drivers of oncogenesis.
Going forward, key research priorities include better understanding the origins of metabolic dysfunction in cancer, determining which alterations are causative versus correlative, and optimizing therapeutic targeting of cancer metabolism. Developing combinations of metabolic interventions with chemotherapy, radiation, and emerging targeted therapies is imperative. There is also great interest in elucidating connections between dysregulated cancer cell metabolism and the immune microenvironment.
In conclusion, while the metabolic theory requires ongoing evaluation, the cumulative evidence suggests that targeting altered energy metabolism in cancer warrants equal attention as targeting genomic instability. Metabolic dependencies and liabilities represent a vast frontier in cancer research that may ultimately yield transformative clinical breakthroughs. The metabolic theory of cancer thus opens promising and provocative new avenues for exploration.
https://phys.org/news/2023-09-exploring-mind-mitochondria.amp
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2845135/ https://www.mdpi.com/1422-0067/23/3/1155 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8467939/ https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/1743-7075-7-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2849637/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7667517/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4762924/